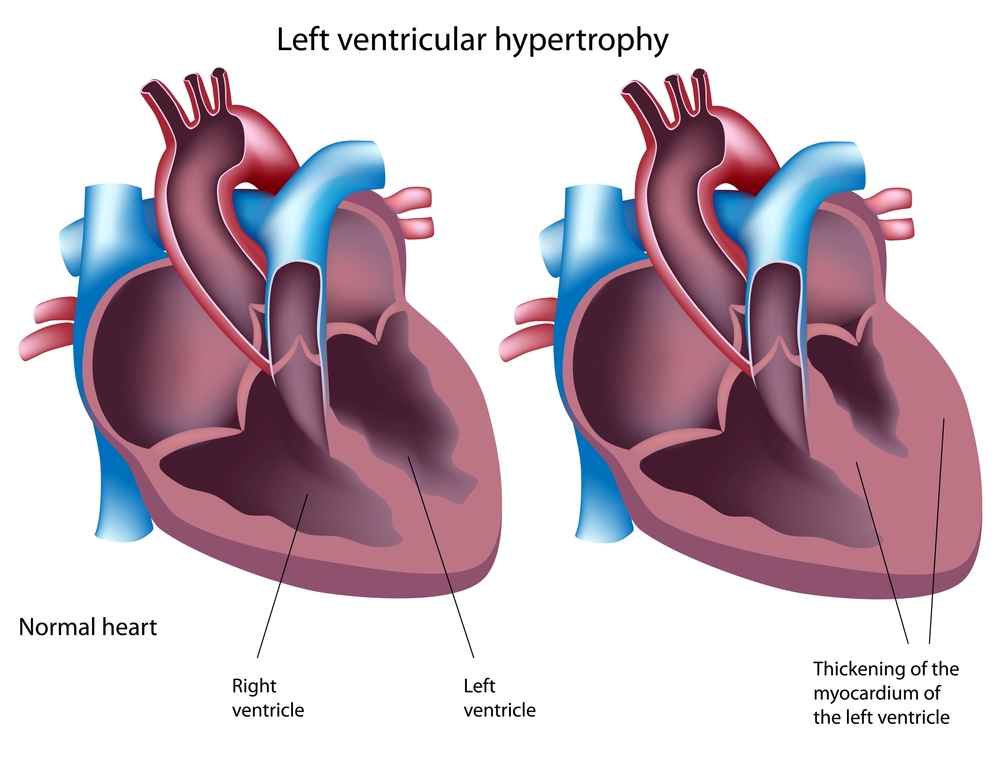
Dear Dr. Scally, Can you help me understand the relationship between anabolic steroids and the enlargement of the heart and the relative risks arising from the steroid-induced increase in heart size? I am concern because several studies have shown that left ventricular hypertrophy (LVH) occurs in individuals that use anabolic-androgenic steroids (AAS).
LVH in athletes is generally considered to be benign physiological LVH as opposed to the dangerous pathological LVH. Physiological LVH would include both anaerobic as well as aerobic training; the adaptation appears to be harmless and regresses over time when training is discontinued.
However, it seems as if the eccentric LVH from aerobic training is more beneficial since it causes an increase in hole diameter, relaxation, and elasticity as opposed to the concentric LVH from anaerobic training (e.g. resistance training) which may actually decrease hole diameter while simultaneously increase size, stiffness, and contraction. Is this true?
Pathological LVH is usually due to long-term uncontrolled hypertension (HTN) although it is very rarely caused by a pre-existing genetic condition known as hypercaridopmyopathy (HCM). Pathological LVH is a risk factor for myocardial infarction (MI), stroke, sudden cardiac death, and congestive heart failure (CHF). So, anything that causes pathologoical LVH should clearly be avoided.
Do you know why AAS causes LVH and what type of LVH it causes? Is it due to androgen receptor (AR) activation in the heart? Is it more likely to be concentric since most bodybuilders and powerlifters, drug-free or natural, already have concentric LVH due to the nature of their training routines?
The statements raise a number of questions all which would take volumes to fully answer. In brief, they are the different forms of left ventricular hypertrophy (LVH), physiological vs. pathological, and the forms that arise from physiological LVH. The cardiac morphologic changes regarding LVH include increased left ventricular cavity dimension, wall thickness, and calculated mass. Finally, what effects do AAS administration have upon LVH and can one safely extrapolate form this safety of long-term (life long) AAS use.
Pathological LVH, as you note, occurs after conditions such as myocardial infarction (pressure overload), inflammatory myocardial disease, with idiopathic dilated cardiomyopathy, or with volume overload. Of importance is the relative benefit/risk screening of athletes for Hypertrophic Cardiomyopathy (HCM) since HCM is regarded to be the most common cause of sudden death in young athletes.
The generally accepted clinical definition of hypertrophic cardiomyopathy, independent of age, is a disease state characterized by unexplained LVH associated with a nondilated ventricular chamber, in the absence of another cardiac or systemic disease, which itself would be capable of producing the magnitude of hypertrophy evident in a given patient. The prevalence of HCM in highly trained athletes is extremely rare. Further, structural and functional changes associated with HCM naturally select out most individuals from competitive sports. A small minority of male athletes may exhibit substantial increases in cardiac size that overlap with the phenotypic manifestation of the cardiomyopathies.
Physiological LVH observed in athletes is often associated with morphological changes in the heart, including increases in left ventricular chamber size, wall thickness, and mass. The increase in left ventricular mass as a result of training is called “athlete’s heart.”
The proposed LVH difference, concentric vs. eccentric, is known as the “Morganroth hypothesis.” In 1975, Morganroth and colleagues hypothesized that the cardiac morphological adaptation observed in athletes corresponded with the nature of the hemodynamic stimulus imposed on the ventricles during repeated exercise bouts.
Endurance training purportedly leads to an eccentric form of cardiac hypertrophy, principally characterized by increased left ventricular (LV) cavity dimension with a proportional increase in wall thickness, and thus LV mass (LVM), as a consequence of prolonged repetitive volume overload. There is an unchanged relationship between left ventricular wall thickness and left ventricular radius (i.e., ratio of wall thickness to radius).
In contrast, strength training is supposedly associated with a concentric form of hypertrophy where increased ventricular wall thickness, with no change in cavity size, underpins the elevated LVM as a consequence of the high systemic arterial pressure overload produced during strenuous resistive exercise. Strength-trained athletes are presumed to demonstrate concentric left ventricular hypertrophy, which is characterized by a changed, increased, ratio of wall thickness to radius.
The “Morganroth hypothesis” has been broadly adopted in the scientific and medical literature, partly as a consequence of a large body of cross-sectional evidence suggesting that endurance athletes have greater cavity dimensions than control subjects or resistance athletes. However, in conflict with the “Morganroth hypothesis,” several studies suggest that LV wall thickness is increased more in endurance, than strength-trained athletes and others have reported no morphological changes in resistance-trained athletes.
The controversial data may reflect variability in the training stimuli, with little obvious attempt to quantify these issues in previous research; more sensitive technologies, such as magnetic resonance imaging, are now being employed for the assessment of cardiac morphology; and the process of scaling (or normalizing) cardiac size for between-subject differences in body size and composition. These considerations emphasize the limitations of the predominance of cross-sectional comparisons in the available literature, which assume that differences between groups are due to a training effect per se rather than other between-subject differences. There are currently limited longitudinal data available to comment on the effects of different modalities of exercise training on LV cavity dimension and wall thickness.
In summary, significant caveats related to cross-sectional literature, the relative insensitivity of echocardiographic measurements and the paucity of evidence from longitudinal exercise training studies, warrant ongoing research to verify the “Morganroth hypothesis.” Currently, there is insufficient high-quality extant evidence to endorse the “Morganroth hypothesis” of differential adaptation to aerobic and resistance training.
Athlete’s heart is generally regarded as a benign increase in cardiac mass, with specific circulatory and cardiac morphological alterations, that represents a physiological adaptation to systematic training. Extreme LV remodeling evident in some highly trained athletes has intuitively raised a concern of whether such exercise-related morphological adaptations are always innocent. There is increasing recognition of the impact that prolonged conditioning has on cardiac remodeling, which may eventually mimic certain pathological conditions with the potential for sudden death or disease progression. Studies show ~15% of highly trained athletes show striking LV cavity enlargement, with end-diastolic dimensions similar in magnitude to that evident in pathological forms of dilated cardiomyopathy.
Overall, athlete’s heart demonstrates normal systolic and diastolic cardiac functions. There is no evidence at present showing that athlete’s heart remodeling leads to long-term disease progression, cardiovascular disability, or sudden cardiac death. The possibility that persistence of extreme remodeling after prolonged and intensive conditioning will ultimately convey deleterious cardiovascular consequences to some athletes is perhaps unlikely but at this time cannot be excluded with certainty.
One might expect AAS exposure to be associated with an exaggerated LV hypertrophic response to any other hypertrophic stimulus. In one very small study, several years after discontinuation of anabolic steroid abuse, strength athletes still showed a slight concentric left ventricular hypertrophy in comparison with AAS-free strength athletes. LVH is an independent risk factor for cardiovascular mortality and (through whatever mechanism) one might anticipate an excess cardiovascular mortality among AAS users in whom LVH occurs. Such data must nonetheless be treated with caution.
So, in your opinion, do you feel that there may be any reason to worry about LVH triggered by long-term AAS use?
At this time the evidence does not show a heightened concern for LVH, particularly at the doses cited in your post. There are no studies demonstrating an association between AAS use and cardiovascular morbidity and mortality. There are a number of anecdotal reports that must be read and interpreted with caution. In my opinion, since these questions are unresolved and other considerations that must be included regarding long-term AAS use, I would recommend against their use in this manner.
My next question is, if AAS induced LVH is not harmful, then would it be okay to stay on a low dose testosterone enanthate (TE) cycle, say 200mg/wk year round, OR 100mg/wk of TPP/NPP combo year round, to keep all my muscular gains? Then do a high dose 12wk @ 800mg/wk Primobolan cycle 1 time a year when I am ready to put on an extra 5-10lbs of dry tissue gains?
If LVH from AAS use is nothing to worry about, is there a downside to my low dose TE OR TPP/NPP year round? I know that there are some individuals that have to be on some type of high-dose AAS 24/7 for many years and even decades, examples being Jose Canseco, Hulk Hogan, and Superstar Billy Graham, with each of these individuals not having any type of heart related ailment that I am currently aware of. On the other hand though, the autopsy report of Eddie Guerrero noted that one of his reasons for death was acute heart failure, so I don’t know if this may have been attributed to AAS induced LVH or not.
Your question makes an assumption, which actually exposes the reason for your post! Since this assumption requires a leap in faith and disregards all other considerations to take into account with long-term AAS use, I do not think that any amount of evidence regarding the adverse effects of AAS use will deter you. In my opinion, even if one was to assume that “AAS induced LVH is not harmful,” there is little to support your idea of AAS use.
About the author
The research of Michael Scally focuses on returning individuals to normal physiology after the discontinuation of anabolic steroids. Dr. Scally has presented his medical protocol for the treatment of Anabolic Steroid Induced Hypogonadism before the Endocrine Society, American Association of Clinical Endocrinologists, American College of Sports Medicine, and International Workshop on Adverse Drug Reactions and Lipodystrophy in HIV. Dr. Scally is the author of "Anabolic Steroids - A Question of Muscle: Human Subject Abuses in Anabolic Steroid Research."
Leave a Reply
You must be logged in to post a comment.