Introductory Physiology and Pharmacology of Androgens
Endogenous androgens are well known for their many functions in promoting sexual differentiation and the induction of the male phenotype. In the male, the two endogenous androgens most active in promoting these effects are testosterone (T) and dihydroxytestosterone (DHT). T is the most quantitatively important androgen in systemic circulation while DHT is the most abundant cellular metabolite and most potent androgen in most androgen sensitive tissues (excluding skeletal muscle; Mainwaring 1977).
The physiological effects of androgens have been discussed since the 1930’s when several investigators observed that the injection of male urinary extracts into dogs not only promoted androgenic effects on the canine reproductive tract but also caused nitrogen retention or an anabolic effect (Kochakian and Mrulin 1935). Since then, much information has been gathered about the various anabolic and androgenic effects of exogenous androgens on human physiology (Braunstien 1997). During fetal development androgens are important in the appropriate differentiation of the internal and external male genital systems. Later, during puberty, androgens mediate growth and functional integrity of the scrotum, epididymis, vas deferens, seminal vesicles, prostate, and penis. During this time androgens also stimulate skeletal muscle growth, growth of the larynx, and stimulate the pubertal growth spurt. Both ambisexual hair growth and sexual hair growth as well as sebaceous gland activity are regulated by androgens throughout the life cycle. Finally, androgens also play many diverse roles in the adult including: behavioral roles (sexuality, aggression, mood, and cognitive function), regulation of spermatogenesis, regulation of bone metabolism, maintenance of muscle mass and muscle function, various effects on the cardiovascular system, and regulation of prostate cancer (Nieschlag and Behre 1998). This list is far from exhaustive as androgens most likely play roles in nearly every organ and cell of the body. As further investigations are conducted, additional physiological effects of endogenous androgens will surely be uncovered.
Although the prior brief discussion has dealt with the physiological effects of the endogenous androgens T and DHT, it must be noted that numerous exogenous steroids have been synthesized in attempts to alter the anabolic to androgenic ratios relative to these two hormones (for a review see Vida 1969). In clinical situations of hypogonadism, T replacement is necessary to replace both the anabolic and androgenic effects of the deficient endogenous androgens. In such situations, T therapy alone is warranted. But in other situations of anabolic deficiency such as catabolic wasting syndromes and administration of glucocorticoids, agents that promote anabolism (nitrogen retention) in the absence of androgenic effects are desirable. Although these agents were originally called “anabolic steroids”, no compound has yet been synthesized that completely dissociates anabolic from androgenic effects. Therefore these agents are still properly termed anabolic androgenic steroids (AAS). Interestingly, subsequent investigations of various anabolic androgenic compounds have demonstrated that many (but not all) of the compounds with very low affinity for the androgen receptor have a more complete dissociation of androgenic and anabolic effects (Saartok et al 1984, Dahlberg et al 1981). Since their relative binding affinities can be as low as 0.01, the mechanism of action of anabolic androgenic steroids might only be directly receptor dependent in a few situations. These situations include extensive intracellular metabolism of the low affinity anabolic androgenic compounds to high affinity compounds or concentration dependent displacement of receptor bound T and DHT by the anabolic androgenic compounds (Gustafsson et al 1984). In addition, even in the absence of viable androgen receptors, these compounds exert androgen specific or anabolic effects in various tissues of the body (Rommerts 1998). These observations may offer indirect evidence for distinct androgen receptor dependent (direct) and androgen receptor independent (indirect) mechanisms of action for the various endogenous and exogenous anabolic androgenic steroids. In fact, Rommerts et al propose that although distinct in some tissues, direct and indirect androgen action may be closely linked in tissues sensitive to both effects (Rommerts 1998). As androgen research becomes more advanced and focuses on examining the androgen receptor, nuclear androgen response elements, and androgen signaling, researchers are getting closer to the desired dissociation of anabolic and androgenic effects.
Androgen Action – Direct and Indirect Mechanisms
Androgen action on target cells remains only partially characterized and understood. Original investigators believed that androgens exerted their effects only through a cytosolic androgen receptor present only in sex-dependent tissues of the body. Today we know the situation to be more complex as both direct or genomic effects as well as indirect or non-genomic effects have been uncovered in nearly every tissue of the body. In addition, androgen receptors have been localized in many tissues not thought to be androgen sensitive. Using radioligand binding techniques, biochemical exchange assays, and immunohistochemical techniques, it is clear that androgen receptors are present in both cytosolic as well as nuclear cellular compartments (Sar et al. 1990).
Although androgens possess both genomic (direct) and non-genomic (indirect) actions, it has been thought that the majority of their action is through direct activation of DNA transcription via high affinity interactions with intracellular androgen receptors (AR). At least it is though so because these interactions have been studied in the most detail. Although receptor dependent interactions may ultimately turn out to be quantitatively most important, as androgen receptor independent actions continue to be uncovered, the importance of these non-genomic interactions may shed new light on androgen’s effects.
It has been demonstrated that some androgen sensitive tissues do not contain nuclear androgen response elements (ARE). In addition, other androgen sensitive tissues do not contain viable intracellular androgen receptors due to AR insensitivity, the absence of AR, or AR blockade. As a result, it has been hypothesized that endogenous androgens (T and DHT for example) may act indirectly on cells without the presence of an AR. To this end, it is thought that androgens might can act as mediators of secondary transcription factors; that they might act in the regulation of autocrine and paracrine mediators of gene expression; or that they might influence the secretion of other hormones that mediate androgen effects in distant tissues (Verhoeven and Swinnen 1999). In addition it is thought that some of these effects may be the result of plasma protein bound androgen interaction with extracellular receptors (Rommerts 1998). Some of the postulated non-genomic, AR-independent effects of androgens include:
- increases in both liver derived and locally produced IGF-I and IGF-I mRNA (Arnold et al 1996, Mauras et al 1998)
- displacement of glucocorticoids from the glucocorticoid receptor and interference of glucocorticoid binding to glucocorticoid response elements (Hickson et al 1990, Danhaive and Rousseau 1986, Danhaive and Rousseau 1988)
- the release of several autocrine “andromedins” including androgen induced growth factor, schwannoma-derived growth factor, keratinocyte growth factor, and fibroblast growth factor, to name a few (Tanaka et al 1992, Sonoda et al 1992, Yan et al 1992)
- transmembrane influx of extracellular calcium (Koenig et al 1989, Lieberherr and Grosse 1994, Steinsapir et al 1991)
- activation of extracellular signal-related kinase cascades via binding to a yet unidentified extracellular receptor (Peterziel 1998)
Although the indirect androgen actions discussed above are still subject to speculation, the evidence for androgen receptor independent action is becoming more impressive. Direct androgen action, on the other hand, is well characterized.
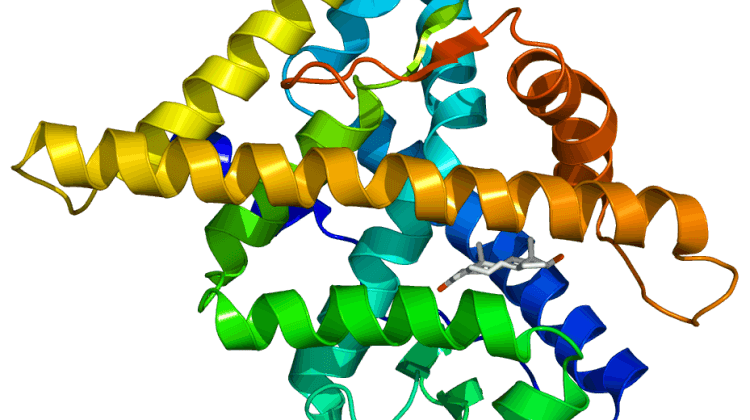
There is however some ambiguity as to whether androgen binds the AR in the cytosol or in the nuclear membrane. Regardless, the AR is typically bound to heat shock protein 90 that maintains the AR inactive state and the AR hormone binding affinity (Fang et al 1996). Upon binding however, direct androgen action is initiated as inhibitory heat shock proteins are released from the androgen receptor. The AR is then phosphorylated and undergoes a conformational change necessary for translocation and dimerization (Grino et al. 1987). Although in the wild-type receptor, this ligand binding is necessary for transcriptional activity, one in vivo receptor with a deleted ligand binding domain does posess transcriptional activity. This may indicate that the unliganded binding domain is actually a repressor of receptor action due to conformational constraints in the unbound receptor possessing the ligand binding domain (Jenster et al 1991). Once in the nucleus (either by direct binding there or by translocation), the phosphorylated receptor is dimerized and binds to a DNA androgen response element (ARE). The hormone response element, which is also bound by other hormone receptors from this family, is a 15 base pair sequence responsible for transcription initiation. Once bound, other transcription regulating proteins or co-activators may also bind the AR-ARE complex to stabilize the promoter of the regulated gene (Shibata et al 1997, Kang 1999). Such co-activators include proteins such as ARA 54, ARA 55, ARA 70, ARA 160 (Yeh et al 1996, Hsiao et al 1999). This binding of such co-factors ultimately results in the regulation of transcription rate. The resultant mRNA from androgen dependent transcription is then processed and transported to ribosomes where it is translated into proteins that can alter cellular function. Although the above mechanism is by far the most predominant, in some tissues there is evidence for a ligand-independent dependent activation of transcriptional activity via the AR. As mentioned above, an unliganded receptor with a deletion of the ligand binding domain may possess activity. This indicates activity in the absence of ligand binding. In addition, growth factors (insulin-like growth factor, keratinocyte growth factor, and epidermial growth factor) as well as protein kinase A activators might be able to induce a transcriptionally active AR in the absence of ligand binding (Culig et al 1995, Nazareth and Weigel 1996). Some of these ligand independent transcription activators may act via influencing the AR phosphorylation state.
The Androgen Receptor
The androgen receptor is a member of the steroid receptor family of nuclear transcription factors. This family is a group of structurally related nuclear transcription factors that mediate the action of steroid hormones. The steroid receptor family includes three other receptors including the glucocorticoid receptor, the mineralocorticoid receptor, and the progesterone receptor (Beato 1989). Although there are several regions of each receptor that are heterologous, the ligand-binding and DNA-binding domains are surprisingly highly conserved (Sheffeild-Moore 2000). In addition to their structural homology, these receptors also are related by their ability to activate gene transcription via the same DNA hormone response element (Quigley et al 1995).
There are two characterized forms of the androgen receptor. The first, and predominant form, is a 110-114 kDa protein of 910-919 amino acids (Jenster et al 1991, Wilson et al 1992, Liao et al 1989). The second is a smaller 87 kDa protein of about 720-729 amino acids in length that makes up only about 4-26% of the detectible androgen receptors located in varying tissues (Wilson and McPhaul 1996). The relevance of this second form of receptor is unknown, but the full-length receptor has been well-characterized. The isolation and characterization of this form of the human androgen receptor cDNA has allowed for sequencing of its amino acid constituents (Chang et al 1989).
The human androgen receptor is a single polypeptide comprised of four discrete functional domains (Quigley 1998).
The A/B region is the N-terminal domain of the AR and comprises over half of the receptor protein (residues 1-537). Within this domain is a transcription activation region and several regions of homopolymeric amino acid stretches that may be important in transcriptional regulation. These amino acid stretches may also be important in interactions with other regions of the receptor protein and in determining the three-dimensional structure of the receptor. Among the four members of the steroid receptor family, this region is poorly conserved both in length and sequence similarity (Evans 1988). The C region of the AR (residues 559-624) is the DNA binding domain. This region is composed of two folded “zinc fingers” which each binding one zinc ion. The first zinc finger is responsible for recognition of the target DNA sequence while the second stabilizes DNA-receptor interaction by contact with the DNA phosphate backbone (Freedman 1992, Berg 1989). Between members of the steroid receptor family, this region is the most highly conserved. At the overlap between the between the C and D regions, there is a nuclear targeting sequence (amino acids 617-633) that is responsible for androgen dependent translocation from the cytosol to the nucleus (Jenster 1993). The D region, or hinge region (residues 625-669), seems to be responsible for androgen dependent conformational changes of the AR. In addition, one of the AR phosphorylation sites is located in this region (Zhou et al 1995). Finally, the E region is the C-terminal domain of the androgen receptor and is responsible for ligand binding. This region consists of about 250 amino acids (residues 670-920) and functions in specific, high affinity binding of androgens. This region is also thought to be the binding site for inhibitory proteins such as the 90 kDa heat shock protein that resides on the inactivated AR. Transcriptional co-activators may also reside here (Jenster 1991).
The AR, as described above, has been identified in a vast array of genital and non-genital tissues using several techniques including northern and western blot analysis as well as immunohistochemical techniques. Most recently, immunohistochemical techniques have become the predominant method of characterization of both cellular and subcellular distribution of the AR due to the sensitivity, specificity, and ease of the method (Ruizeveld De Winter et al 1991, Kadi et al 1999, Sar et al 1990). Using immunohistochemical techniques, the AR has been clearly demonstrated in nearly all tissues (Janssen et al 1994, Kimura et al 1993, Takeda et al 1990). As mentioned earlier, despite characterization in both the cytosol and nucleus, the exact location of ligand binding is not yet clear. The predominant model (shown above in figure 1) however suggests that the cytosolic AR is inactive until it binds ligand. At this point it it undergoes an appropriate conformational change and it is transolcated to the nucleus via the nuclear targeting sequence (residues 617-633; Grino et al 1987, Jenster et al 1993, Zhou et al 1994). At this point, it is able to undergo binding to the androgen response element.
Based on early studies, the AR has been identified as a high affinity, low capacity receptor. Saturation binding analyses done using the androgen receptor radiolabelled ligands [3H]-T, [3H]-methyltrienolone (MT), and [3H]-DHT have shown saturability and therefore have been analyzed using scatchard plots corrected for nonspecific binding. The results of such investigations have been difficult to interpret however due to several confounding variables. First, since the amount of AR protein seems to be very low, small experimental errors will translate into large statistical errors. In addition, a significant amount of non-specific binding is found in AR experiments (Snochowski et al 1979). If this binding is not corrected for, then experimental errors could again be large. Also, androgens (especially T and DHT but not MT) are subject to several metabolic enzyme systems that differ between tissues. If uncontrolled, these metabolic pathways could also confound results. For example, measurements of apparent DHT binding to the AR may be underestimated due to metabolic conversion to androstanediols that do not bind to the receptor while the measures for apparent T binding could be overestimated due to formation of DHT which will bind strongly to the receptor (Michel and Baulieu 1980). Finally, since Kd values and Bmax values for the AR are variable with species, sex, age, and androgen levels, controlling all variables relevant to the AR presents a difficult proposition (Stahl et al 1978). As a result of the potential confounds discussed, Kd values from 0.074nM up to 6.4nM and Bmax values from 1-30 fmol/mg protein have been reported for the AR in various tissues using different radiolabelled ligands. With this said, close inspection of the published literature reveals that since different radiolabelled ligands have been used in the research, since different cytosolic preparations have been employed, and since different populations and species have been used, it only stands to reason that variable results have been obtained.
In this review, I will discuss binding affinity and capacity in one tissue (skeletal muscle) to simplify the discussion. Since skeletal muscle does not possess significant amounts of the enzyme responsible for the conversion of T to DHT (5alpha reductase), T is the predominant AR ligand. In research examining the skeletal muscle AR using labeled T, the lack of metabolic conversion to DHT helps to eliminate one potential confound. Other metabolic conversions using the 3alpha- and 3beta-hydroxysteroid dehydrogenases remain and can only be controlled by the addition of ammonium sulfate to the cytosolic preparation to eliminate the activity of these enzymes (Michel and Baulieu 1980). These two precautionary measures, however are incomplete and the synthesis of methyltrienolone (17 alpha-methyl-3-oxo-estra-4,9,11-trien-17 beta-ol), which binds to the AR with the same affinity as T yet is not metabolizable, was of greta value to AR binding studies. The use of labeled MT therefore has added another element of control to AR studies.
Preliminary work by Michel and Baulieu using [3H]-T and [3H]-androstanolone (DHT) ligands in enzyme-free preparations of castrate male and female rat quadriceps femoris yielded similar Kd values for both ligands of approximately 0.70nM (Michel and Baulieu 1980). These values are similar to several other reports of T affinity in skeletal muscle. In another investigation using rat thigh homogenates prepared with [3H]-T, Kd values of approximately 1nM and Bmax values of 15-30 fmol/mg protein were found (Michel and Baulieu 1974). The Bmax values in this experiment are higher than those reported anywhere else in the literature for skeletal muscle. Krieg et al, using [3H]-androstanolone (DHT) in rat muscle homogenates found a Kd range of 1.4nM to 6.4nM and 0.8-4.2 fmol/mg protein (Krieg 1976). Krieg et al could not explain the reason for differences between their work and the work of Michel and Baulieu but hypothesized that such errors could potentially arise due to the very small amount of receptors in the cytosol as well as the fact that these receptors are very difficult to isolate. Later work by Saatok et al, using the nonmetabolizable [3H]- MT in rabbit skeletal muscle cytosol preparations, found Kd values of 1.25-1.66nM and Bmax values of 2.76-5.18 fmol/mg protein, potentially confirming the work of Krieg (Saatok 1984). Finally, work by Snochowski et al also using [3H]- MT in male and female human skeletal muscle cytosolic preparations has indicated that Kd values for the AR were approximately 0.074-0.7nM (mean of 0.28nM) while Bmax values were 1-4fmol/mg protein (Snochowski et al 1981). From these variable data it is obvious that although the AR is clearly a high affinity and low capacity receptor, useful and consistent quantitative data have not been obtained regarding affinity and capacity in muscle. The differences in this literature again could be due to the different radioligands used in the studies, different ages and androgen levels in the subject populations, and amplified experimental errors due to such small levels of detectible AR protein. To discuss skeletal muscle in relation to the prostate, although variable results have been obtained for prostate tissue as well, Bmax values seem to be about 10fold lower (per mg protein) while Kd values are of a similar magnitude (Ekman et al 1979).
Androgen Metabolism and AR Binding
To further elaborate on the importance of androgen metabolism in the determination of AR levels and, more importantly, in the mechanism of action of androgens, a brief discussion of this subject is in order. T and DHT are the two most potent androgens in the body however their relative importance in different tissues varies. It is known that although the prostate AR can bind both T and DHT, the affinity of the AR for T is only 33% of that for DHT (Grover et al 1975). In contrast, in skeletal muscle and kidney fractions, the binding affinity for T is greater than that for DHT despite affinity for both ligands (Gloyna and Wilson 1969, Bullock et al 1974). T itself is extensively metabolized in most androgen-sensitive tissues. The predominant metabolite in the prostate, for example, is DHT. Important in this metabolic pathway are the relative levels of 5alpha reductase and 3alpha- and 3-beta hydroxysteroid dehydrogenases. Since DHT is the active metabolite in most tissues, high conversion of T to DHT via the 5 alpha reductase pathway and low metabolism of DHT via the 3 hydroxysteroid dehydrogenase pathways is necessary for optimal androgen action (Rommerts 1999). In skeletal musle, on the other hand, 5alpha reductase activity is low while 3alpha- and 3-beta hydroxysteroid dehydrogenase activity is higher leading to a predomination of T and other inactive metabolites. In fact, in skeletal muscle, less than 5% of T is metabolized (Minguell and Sierralta 1975). This is optimal due to the fact that in skeletal muscle, the AR has a higher affinity for T than for DHT. Interestingly, despite the differences between the metabolic pathways for T as well as the differences in affinities for various T metabolites, the AR appears to be nearly identical in structure across androgen sensitive tissues. The differences in androgen action between tissues is now thought to be due to DNA response elements as well as specific co-activators or repressors present in the different tissues.
Conclusions
In conclusion, this review has discussed several relevant topics in androgen pharmacology, physiology, and receptor theory. Although much is yet to be discovered regarding androgen mechanism of action, the androgen receptor, regulation of androgen receptor mediated transcription, and control of the androgenic and anabolic effects of testosterone and its metabolites, new discoveries are rapidly being reported. With investigations currently being conducted to examine androgen receptor co-activator proteins as well as androgen response element functions in a wide spectrum of tissues, manipulation of some of the diverse actions of androgens can be postulated. And these discoveries may contribute to the holy grail of androgen research; successful dissociation of the anabolic and androgenic affects of androgens.© 2002 – 2003 Science Link, Inc. All rights reserved. Reprinted with permission.
References
1) Arnold, A.M. et al. Journal of Endocrinology. 150, 291-399, 1996.
2) Beato, M. Cell. 56, 335-344, 1989.
3) Berg, J. Cell. 57, 1065-1068, 1989.
4) Braunstien, G.D. in Basic and Clinical Endocrinology, Greenspan F.S. and Strewler G.J. eds. Appleton and Lange, Stanford CT, 403-433, 1997.
5) Bullock, L.P. et al. Endocrinology. 94, 746-748, 1974.
6) Chang, C. et al. Proc Natl Acad Sci USA, 85: 7211-7215, 1988.
7) Christiansen, K. in Testosterone Action, Deficiency, and Substitution, Nieschlag, E. and Behre, H.M. eds. Springer-Verlag, New York, 107-142, 1998.
8) Culig, Z. et al. World J Urol. 13, 285-289, 1995.
9) Dahlberg, E. et al. Endocrinol. 108, 1431-36, 1981.
10) Danhaive, P.A. and Rousseau, G.G. J Steroid Biochem Mol Biol. 24, 481-487, 1986.
11) Danhaive, P.A. and Rousseau, G.G. J Steroid Biochem Mol Biol. 29, 575-581, 1988.
12) Ekman, P. et al. J Clin Endo Met. 49, 205-215, 1979.
13) Evans, R.M. Science. 240, 889-893, 1988.
14) Fang, Y. et al. J Biol Chem. 271 (45), 28697-28702, 1996.
15) Freedman, L.P. Endocr Rev. 13, 129-145, 1992.
16) Gloyna, R.E. and Wilson, J.D. J Clin Endocrinol. 29, 970-973, 1969.
17) Grino, P.B. et al. Endocrinol. 120, 1914-1920, 1987.
18) Grover, P. and Odell, W. J Steroid Biochem. 6, 1373-1379, 1979.
19) Gustafsson, J. et al. In Hormones and Cancer, Gurpide, E. et al. eds. Alan R. Liss, Inc. New York, 261-290, 1984.
20) Hickson, R.C. et al. Med Sci Sports Exerc. 22, 331-340, 1990.
21) Hsiao, P.W. J Biol Chem. 32, 22373-22379, 1999.
22) Janssen, P.J. et al. J Histochem Cytochem. 42, 1169-1175, 1994.
23) Jenster, G. et al. Biochem J. 293, 761-768, 1993.
24) Jenster, G. et al. Mol Endocrinol. 5, 1396-1404, 1991.
25) Kadi, F. et al. Histochem Cell Biol. 113, 25-29, 2000.
26) Kang, H.Y. J Biol Chem. 274 (13), 8570-8576, 1999.
27) Kimura, N. et al. J Histochem Cytochem. 41, 671-678, 1993.
28) Kochakain, C.D. and Murlin, J.R. J Nutr. 10, 437, 1935.
29) Koenig, H. et al. Circ Res. 64, 415-426, 1989.
30) Krieg, M. Steroids. 28(2), 261-274, 1976.
31) Laio, S. et al. J Steroid Biochem. 34, 41-51, 1989.
32) Lieberherr, M. and Gross, B. J Biol Chem. 269, 7219-7223, 1994.
33) Mainwaring, W.I.P. et al. The Mechanism of Action of Androgens. Verlag New York, 8-10, 1977.
34) Mauras, N. et al. J Clin Endocrinol and Metab. 83: 1885-1892, 1998.
35) Michel, G. and Baulieu, E.E. CR Acad Sci Paris. 279, 421, 1974.
36) Michel, G. and Baulieu, E.E. Endocrinol. 107 (6) 2088-2098, 1980.
37) Minguell, J.J. and Sierralta, W.D. J Endocr. 65, 287-315, 1975.
38) Nazareth, L.V. and Weigel, N.L. J Biol Chem. 271, 19900-19907, 1996.
39) Nieschlag, E. and Behre, H.M. Testosterone Action, Deficiency, and Substitution. Springer-Verlag, New York, 1998.
40) Peterziel, H. et al. In Verhoeven, G., and Swinnen, J.V. Molecular and Cellular Endocrinology. 151, 205-212, 1999.
41) Quigley, C. et al. Endocr Rev. 16, 271-321, 1995.
42) Quigley, C.A. in Testosterone Action, Deficiency, and Substitution, Nieschlag, E. and Behre, H.M. eds. Springer-Verlag, New York, 33-104, 1998.
43) Rommerts, F.F.G. In Testosterone Action, Deficiency, and Substitution, Nieschlag, E. and Behre, H.M. eds. Springer-Verlag, New York, 1-31, 1998.
44) Ruizeveld De Winter, J.A. et al. J Histochem Cytochem. 39, 927-936, 1991.
45) Saartok, T. et al. Endocrinol. 114, 2100-2107, 1984.
46) Saartok, T. Int J Sports Med. 5, 130-136, 1984.
47) Sar, M. et al. Endocrinol. 127, 3180-3186, 1990.
48) Sheffield-Moore, M. Ann Med. 32, 181-186, 2000.
49) Shibata, H. Recent Progress Horm Research. 52, 141-164, 1997.
50) Snochowski, M et al. J Steroid Biochem. 14, 765-771, 1981.
51) Sonoda, H. et al. Biochem Biophys Res Commun. 185, 103-109, 1992.
52) Stahl, F. et al. In Hormones and Brain Development, Dorner, G. and Kawami, M. eds. Elsevier, Amsterdam, 99-109, 1978.
53) Steinspar, J. et al. Biochem Biophys Res Comm. 179, 90-96, 1991.
54) Takeda, H. et al. J Endocrinol. 126, 17-25, 1990.
55) Tanaka, A. et al. Proc Natl Acad Sci. USA 89, 8928-8932, 1992.
56) Verhoeven, G., and Swinnen, J.V. Molecular and Cellular Endocrinology. 151, 205-212, 1999.
57) Vida, J.A. Androgens and Anabolic Agents, Chemistry and Pharmacology. Academic Press, Inc, New York, 77-91, 1969.
58) Wilson, C.M. and McPhaul, M.J. Mol Cell Endocrinol. 120, 1, 51-57, 1996.
59) Wilson, C.M. et al. J Clin Endocrinol Metab. 75, 1474-1478, 1992.
60) Yan, G. et al. Mol Endocrinol. 6, 2123-2128, 1992.
61) Yeh, S. et al. Proc Natl Acad Sci USA. 93 (11), 5517-5521, 1996.
62) Zhou, Z. et al. J Biol Chem. 269, 13115-13123, 1994.
63) Zhou, Z. et al. Mol Endocrinol. 9, 605-615, 1995.
About the author
John Berardi, PhD., received his doctoral degree at the University of Western Ontario. He studied exercise physiology and nutrient biochemistry under renowned sport nutrition researcher Dr. Peter Lemon. His research focused primarily on exercise nutrition; specifically, what to eat before, during and after exercise to optimize performance. He's been an assistant adjunct professor at the University of Texas and a course instructor at Eastern Michigan University, teaching courses in Exercise Science, Nutrient Metabolism, Fitness and Wellness, and Exercise Nutrition.
Leave a Reply
You must be logged in to post a comment.