Estimated reading time: 19 minutes
Table of contents
Introduction
Testosterone replacement therapy is not without side effects, although most are manageable. I’ve been taking testosterone replacement for 16 years and for the most part have had few side effects thanks to careful monitoring. It’s critical that you are monitored for side effects in addition to your testosterone level. Some men may experience one or more side effects that sometimes go unnoticed until it is too late. In part it is the underground, unmonitored use of testosterone that creates so much bad publicity for a very helpful product.
The first step in the proper monitoring of replacement therapy is providing your doctor with a thorough medical history. Appendix A shows a simple and comprehensive medical history form (courtesy of Dr John Crisler, allthingsmale.com). Patients who would like to be proactive can fill out this form and give a copy to their doctor. It is expected that every doctor have a similar form, although most do not ask questions pertinent to sexual function or on the use of androgens. Let your doctor know about all the medications you take so that medication-induced sexual dysfunction can be ruled out before starting testosterone.
I also strongly believe that if a patient goes to the doctor to obtain a Viagra, Cialis or Levitra prescription, the doctor should check the patient’s testosterone blood levels to ensure that it is not the root of the problem. Hypogonadal men may not respond as well to these drugs if their testosterone is not normalized first. Studies combining testosterone and oral sexual enhancement drugs have shown a synergistic effect on sexual benefits. The following suggested guidelines for monitoring testosterone replacement is recommended by several physician groups and practices:
You should be evaluated after the first month of therapy to measure your testosterone blood levels. If your doctor doesn’t ask, let him know about your quality of life. Make sure your doctor is aware of your energy level, mood, and sexual function, as well as any potential side effects (tender breasts, urinary flow decrease, moodiness, and acne).
When using testosterone, your doctor will want to measure total blood testosterone levels right before the next corresponding injection after the first month (it takes a while for the blood levels to stabilize). If testosterone is >700 ng/dl (24.5 nmol/liter) or <350 ng/dl (12.3 nmol/liter), your doctor will adjust the amount or the frequency of your dose. I mentioned this earlier in the book but it bears repeating here: Some men need to have levels above 500 ng/dl to experience any of the expected sexual function benefits from testosterone. It is important to be honest about when your doctor asks you about your sexual performance.
Your doctor will check your hematocrit before starting testosterone, after 3 months and then every year after that. If your hematocrit is above 54%, you may need a therapeutic phlebotomy (read the section “Checking for Increased Blood Thickness (Polycythemia)” for more details.
Be ready to have a digital rectal examination done and a prostatic specific antigen (PSA) blood test drawn prior to starting testosterone, and after 3 months. Once every 6 months after that may not be unreasonable, especially in older men. A PSA over 4 ng/ml can be reason for concern and referral to an urologist. Testosterone replacement needs to be stopped if increases in PSA above normal are observed. Note: at the start of testosterone replacement in older men, when testosterone blood levels are rapidly rising, PSA may also increase. This is especially true when testosterone gels are employed, because they elevate DHT more relative to other options. Once testosterone levels have stabilized PSA drops back down to roughly baseline. It is important to allow “steady state” for testosterone fluctuations to stabilize before measuring PSA; a month or so should be sufficient.
If you start experiencing breast tenderness, pain or growth, ask your doctor to measure your estradiol blood level using the sensitive assay (not the regular test used for women). Normal range for estradiol in men is 14–54 pg/ml (50–200 pmol/liter). Men who have high estradiol can be prescribed estrogen receptor inhibitors (more details in “Avoiding enlarged breasts (gynecomastia)”
Ensuring Prostate Health—No Link Found Between Androgen Levels and Risk for Prostate Cancer
The prostate is a gland that is part of the male reproductive system. Its function is to store and secrete a slightly alkaline (pH 7.29) a milky fluid which usually constitutes 25-30% of the volume of the semen along with spermatozoa. This alkaline fluid seems to neutralize the acidity in the vagina, prolonging the life span of the sperm. Also, the prostate contains some smooth muscles that help expel semen during ejaculation. It also helps control the flow of urine during ejaculation.
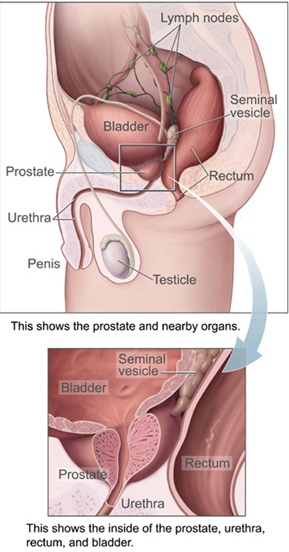
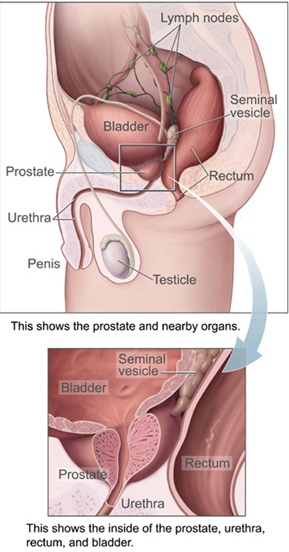
A healthy human prostate is classically said to be slightly larger than a walnut. In actuality, it is approximately the size of a kiwi fruit. It surrounds the urethra just below the urinary bladder and can be felt during a rectal exam.
Prostate cancer
This little gland attracts a great deal of attention in men’s health. One of the major issues is related to cancer. Prostate cancer is one of the leading causes of death in men in the United States. As men age, small hidden prostatic lesions become increasingly common. These may or may not become cancerous. These lesions occur in 30 percent of American men over the age of 45, with the prevalence rising to more than 80 percent for men over the age of 80. Genetic factors and life style conditions such as diet are believed to contribute to this transformation. [Figure 14. The prostate and surrounding organs (Courtesy of Wikipedia.com)].
Doctors use different methods to detect prostate cancer, including prostate-specific antigen (PSA) assays, digital rectal examination (DRE), and transrectal ultrasound. A DRE before starting testosterone replacement therapy and every six months is recommended, especially for men with a family history of prostate cancer or those older than 40 years. Nobody likes having a DRE but your continued good health is worth a few seconds of discomfort. An abnormal rectal exam, a confirmed increase in PSA greater than 2 ng/mL, or PSA of over 4 ng/mL will prompt a health care provider to refer you to a urologist for further evaluation (usually an ultrasound and prostate biopsies).
Admittedly the PSA and the DRE lack sensitivity and specificity. 25 percent of patients with prostate cancer have normal PSA levels (false negatives), while benign prostatic hyperplasia (BPH), a non-cancerous inflammation, may elevate them (false positives). Researchers have found hidden prostatic lesions with needle biopsies in some men with normal PSA level and normal transrectal ultrasound findings. Prostate biopsies are part of routine clinical use of testosterone therapy and are not justified unless a sharp rise in PSA is observed and infections have been ruled out.
There has some been confusion regarding testosterone replacement therapy’s role in PSA elevation or causing prostate cancer. Prostate cancer is initially androgen-dependent so testosterone therapy should not be used by men with prostatic cancer. This does not mean that it causes cancer. A huge pooled analysis of data from 18 studies (consisting of 3,886 men with prostate cancer and 6,438 controls), published in the February 6, 2008 issue of the Journal of the National Cancer Institute found that blood levels of androgens and other sex hormones do not seem to be related to an increased risk for prostate cancer. In short, testosterone therapy does not appear to cause prostate cancer but it can make it worse.
Prostate infection
Another health concern is prostatitis or prostate infection. This is common in aging men and can be a leading cause of an elevated PSA. Your doctor will want to check you for an infection if your PSA unexpectedly increases by checking your urine for white blood cells. If they are high, he may refer you to an urologist who would induce a discharge from your penis to look at it under the microscope. Don’t ask me how the urologist does it, ask the urologist!
Benign prostatic hyperplasia
A common health condition is benign prostatic hyperplasia or BPH. It is estimated to occur in 50 percent of men older than 50 years. Increased frequency of urination, frequent trips to the bathroom at night, incomplete voiding, and urgency to urinate indicate possible prostatic inflammation. BPH does not necessarily lead to increased rates of prostate cancer. There have been no prospective, controlled, long-term studies on the effects of testosterone administration on either the development or the progression of BPH. One open label, one-year study that measured prostate size using ultrasound foundnoincrease during testosterone replacement therapy, suggesting that the treatment does not cause BPH. Whether testosterone treatment worsens asymptomatic BPH has not been established. Some individuals are more prone to prostatic inflammation when using testosterone.
Another study was conducted by Dr. Michael D. Trifiro at Moores UCSD Cancer Center in San Diego. Dr. Trifiro observed 158 men for 20 years to determine the correlation between serum sex hormones and lower urinary tract symptoms (reduced urinary flow, urgency, and other symptoms associated with BPH). The researchers found no significant associations of total testosterone, estradiol (E2)), testosterone: E2ratio, DHT, or dehydroepiandrosterone with lower urinary track symptoms or with any measured hormones(published inBJU Internationalin December 2009).
Tesosterone replacement therapy is not contraindicated in those with BPH. Men with BPH who need to start testosterone replacement should be observed very closely. The first symptom that worsens with increased BPH is restricted urinary flow and urgency, especially during sleep hours. Many urologists are successfully prescribing medications to ease those symptoms and improve urinary flow in men with BPH. Finasteride (brand name: Proscar), which was approved by the FDA in 1992, inhibits production of dihydrotestosterone (DHT), which is involved with prostate enlargement. Its use can actually shrink the prostate in some men. However, many men using Proscar complain of erectile dysfunction (DHT receptors may be involved in healthy erctions). For men who experience this side effect, other medications may be of help. Proscar has also been found to decrease the risk of prostate cancer in men by 25 percentover aseven year period. More studies are ongoing.
The FDA approved the drugs terazosin (brand name: Hytrin) in 1993, doxazosin (Cardura) in 1995, and tamsulosin (Flomax) in 1997 for the treatment of BPH. All three belong to the class of drugs known as alpha blockers. They work by relaxing the smooth muscle of the prostate and bladder neck to improve urine flow and to reduce bladder outlet obstruction.
Terazosin and doxazosin were developed first to treat high blood pressure. Tamsulosin is the first alpha-blocker developed specifically to treat BPH. The main side effects of these drugs are nasal congestion, lowered blood pressure, and rash or itching. Most men using them report fast improvements in their urine flow within one to three days. They end up not having to get up in the middle of the night to urinate, so they sleep better and feel less fatigued during the day.
The most common nonprescription agent used to alleviate symptoms of BPH is the over-the-counter herb saw palmetto (Serenoa repens). Extracted from the berry of the saw palmetto shrub, this substance is thought to inhibit 5-alpha reductase (5-·R), thus blocking the conversion of testosterone into DHT, which is responsible for stimulating growth of the prostate gland.
Saw palmetto is generally well tolerated; side effects are infrequent, but include headache and gastrointestinal upset. No known drug interactions are associated with the use of this herb. Some studies found that saw palmetto led to an increase in urine flow rate in men with BPH compared with placebo, with effects comparable to finasteride.
One randomized, double-blind, placebo-controlled study followed men with BPH who took standardized saw palmetto extract 160 mg or placebo twice daily for one year. There was no significant difference found between the saw palmetto and placebo groups in standardized objective urinary symptoms. The incidence of side effects was similar in the two groups. These results cast considerable doubt on the effectiveness of saw palmetto for the treatment of BPH.
Patients who cannot tolerate BPH medications are now using emerging techniques like lasers to vaporize obstructing prostate tissue (www.greenlighthps.com). Talk to your urologist about this if you’re interested.
PERSONAL COMMENT: After using testosterone for 17 years, I started to develop a weak urine flow. My doctor gave me prescriptions for several alpha blockers (Uroxatral, Flomax, etc). They worked great but I experienced a rash with each one. My urologist found a prostate infection, which he treated with antibiotics. The infection seemed to linger for months. I then received an ultrasound of my prostate. This test showed that my prostate was not enlarged. Instead it showed that a calcification, caused by a chronic prostatic infection, was blocking my urine flow through my prostate. I got the green light laser procedure done to open up my urethra. It worked great. So, what may seem like BPH may not be! Prostatic infections often go untreated for months since in many cases we may not have symptoms.
Checking for Increased Blood Thickness (Polycythemia)
In addition to increasing muscle and sex drive, testosterone can increase your body’s production of red blood cells. This hemopoietic (blood building) effect could be a good thing for those with mild anemia. An excessive production of red blood cells is called polycythemia; it’s not a good thing. With polycythemia the blood becomes very viscous or “sticky” making it harder for the heart to pump. High blood pressure, strokes, and heart attacks can occur. This problem is not that common in men taking replacement doses of testosterone but more common in those taking higher bodybuilder doses.
It’s important to have your doctor check your blood’s hemoglobin and hematocrit.. Hemoglobin is the substance that makes blood red and helps transport oxygen in the blood. Hematocrit reflects the proportion of red cells to total blood volume. The hemoglobin and hematocrit should be checked before starting testosterone replacement therapy, at three to six months and then annually. A hematocrit of over 54 percent should be evaluated. Discontinuation of testosterone may be necessary but there is another option.
Many patients on testosterone replacement who experience polycythemia do not want to stop the therapy due to fears of re-experiencing the depression, fatigue and low sex-drive they had before starting treatment. For those patients, therapeutic phlebotomy may be the answer. Therapeutic phlebotomy is very similar to what happens when donating blood, but this procedure is prescribed by your physician as a way to bring down your blood levels of hematocrit and viscosity.
A phlebotomy of one pint of blood will generally lower hematocrit by about 3 percent. I have seen phlebotomy given weekly for several weeks bring hematocrit from 56 percent to a healthy 46 percent. I know physicians who prescribe phlebotomy once every six weeks because of an unusual response to testosterone replacement therapy. This simple procedure is done in a hospital blood draw facility and can reduce hematocrit, hemoglobin, and blood iron easily and in less than one hour. Unfortunately, therapeutic phlebotomy can be a difficult option to get reimbursed or covered by insurance companies. Your doctor may need to write a letter of medical necessity for it. If you are healthy and without HIV, hepatitis B, C, or other infections, you could also donate blood at a blood bank (a great way to help others!).
The approximate amount of blood volume that needs to be withdrawn to restore normal values can be calculated by the following formula, courtesy of Dr. Michael Scally, an expert on testosterone side effect management. The use of the formula includes the assumption that whole blood is withdrawn. The duration over which the blood volume is withdrawn is affected by whether concurrent fluid replacement occurs.
Volume of Withdrawn Blood (cc)=
Weight (kg) × ABV×[Hgbi– Hgbf]/[(Hgbi+Hgbf)/2]
Where:
ABV = Average Blood Volume (default = 70)
Hgbi(Hcti) = Hemoglobin initial
Hgbf(Hctf) = Hemoglobin final (desired);
So, for a 70 kg (154 lbs) man (multiply lbs x 0.45359237 to get kilogram) with an initial high hemoglobin of 20 mg/mL who needs to have it brought down to a normal hemoglobin of 14 mg/mL, the calculation would be:
CC of blood volume to be withdrawn = 75 x 70 x [20—l4]/[(20 + l4)/2]
= 75 x 70 x (6/17) = approximately1850cc;
One unit of whole blood is around350 to 450 cc; approximately4 units of blood need to be withdrawn to decrease this man’s hemoglobin from 20 mg/mL to 14 mg/mL.
The frequency of the phlebotomy depends on individual factors, but most men can do one every two to three months to manage their hemoglobin this way. Sometimes red blood cell production normalizes without any specific reason. It is impossible to predict exactly who is more prone to developing polycythemia, but men who use higher doses, men with higher fat percentage, and older men may have a higher incidence.
Some doctors recommend the use of a baby aspirin (81 mg) a day and 2,000 to 4,000 mg a day of omega-3 fatty acids (fish oil capsules) to help lower blood viscosity and prevent heart attacks. These can be an important part of most people’s health regimen but they are not a replacement for therapeutic phlebotomy if you have polycythemia and do not want to stop testosterone therapy. It amazes me how many people assume that they are completely free of stroke/heart attack risks by taking aspirin and omega-3 supplements when they have a high hematocrit.
Although some people may have more headaches induced by high blood pressure or get extremely red when they exercise, most do not feel any different when they have polycythemia. This does not make it any less dangerous. If you are using testosterone on your own you need to let your doctor know. Your physician may already suspect some sort of anabolic use if lab results reveal elevated hemoglobin and hematocrit.
PERSONAL COMMENT: I had polycythemia back in the mid-1990s when I was using supraphysiologic doses of testosterone and nandrolone to reverse my HIV-related weight loss. I required two phlebotomies in six months. My hematocrit and hemoglobin eventually normalized without any reason even when using the same doses of testosterone and nandrolone.
Ensuring Liver Health
I mentioned this before but it is well worth repeating. Contrary to what some physicians may think, injectable and transdermal testosterone have not been known to cause increased liver enzymes. The same cannot be said for over-the-counter supplements that claim to increase testosterone or growth hormone. Not only do most of them not work, but they could increase your liver enzymes to dangerous levels. This problem has been reported in the past to the FDA. I warn people all the time to be careful about their use. It is always good to check your liver enzymes when blood work is done since it is a cheap test and highly useful in detecting toxicities caused by medications or supplements you may be using.
It is the use of oral testosterone and anabolic formulations (except for oral testosterone undecanoate, commonly used in Canada) that can increase liver enzymes. Many men with hepatitis B or C can be safely treated with replacement doses of testosterone without any liver injury if gels, patches or injections are used. I am very concerned that some of these patients may be denied this important therapy due to potential fears and misconceptions. Some studies have shown an increased incidence of hypogonadism, fatigue, and sexual dysfunction in patients with hepatitis.
Some men like to take supplements to protect the liver against the damaging effects of medications, but very limited data is available on their use. Supplements potentially can interfere with medication blood levels; very little is known about supplement-drug interactions. However, I would like to bring up some supplements with data on liver protection:
- Standardized silymarin (milk thistle herb)—160 mg/three timesday
- Evening primrose oil—1,300 mg/three times/day
- Alpha lipoic acid– 100 – 300 mg/three times/dayGlycyrrhizinate Forte –Three or more capsules/day, but this may increase blood pressure.
- N-acetyl cysteine– 600 mg/three times/day
- Selenium– 200 mcg twice a day.
I trust the Jarrow and Super Nutrition brands for most of my supplements. Talk to your doctor before starting any supplements!
Monitoring Blood Pressure
High blood pressure or hypertension is another serious medical condition that can go undetected because it often has no symptoms. It’s referred to as “the silent killer” for this reason. High blood pressure can cause heart attacks, strokes, headaches, ruin your kidneys, erectile dysfunction and shrink your brain.
Before you start testosterone replacement or an exercise program, it is very important to get your blood pressure under control. This is done through diet, stress management, lowering your salt intake and/or the use of medications. It is a good idea to invest in a home-based blood pressure machine. One usually can be purchased at most pharmacy chains and cost under US$50. Some, like the OMRON HEM-780, can measure blood pressure easily and keep track of changes with time. Take measurements twice a day until you gain control of your blood pressure again.
It is important to have your blood pressure measured during the first month of treatment to ensure that it does not increase with testosterone. The good news is that replacement doses are much less associated with this problem. More serious risks for hypertension are associated with the high testosterone doses associated with performance-enhancing use.
NOTE: Some natural ways to decrease blood pressure are decreasing your salt intake, exercising, keeping a normal body weight for your height, managing stress, and engaging in meditation and yoga. “Erection-friendlier” blood pressure medications like ACE (angiotensin converting enzyme) inhibitors, renin inhibitors, ARB’s (angiotensin II receptor blockers), and combinations of them may be required for men who cannot maintain a blood pressure reading under 130/80 mm Hg.
Avoiding Enlarged Breast (Gynecomastia)
Yes, I am talking about breast appearance in men, not women. Gynecomastia is a benign enlargement of the male breast resulting from a growth of the glandular tissue of the breast. It is defined clinically by the presence of a rubbery or firm mass extending concentrically from the nipples. Men who start experiencing this problem complain of pain and tenderness around the nipple area. Gynecomastia is caused by higher than normal blood levels of estradiol, a metabolite of estrogen. As discussed earlier in the book, testosterone can convert into estradiol, DHT, and other metabolites. Men with higher amounts of the enzyme aromatase usually have this problem even at lower doses of testosterone. Growth of this glandular tissue is influenced by a higher fat percentage, older age, excessive alcohol intake, and the use of certain medications. Gynecomastia usually occurs early in testosterone replacement in those who experience this side effect.
In several studies on testosterone replacement, only a very small percentage of people receiving testosterone experience growth of breast tissue. In one HIV-specific study conducted by Dr. Judith Rabkin in New York, she reported that out of 150 men enrolled in the study, two men experienced this adverse reaction. Gynecomastia is much more common among those who use high testosterone doses, such as bodybuilders (they call this “gyno” or “bitch-tits”).
How do you manage gynecomastia if it does occur? Lowering the testosterone dose had not proven helpful for the two patients in Dr. Rabkin’s study. The use of antiestrogens, such as tamoxifen 10 mg twice daily, with lower doses of testosterone has been effective. Gynecomastia can become permanent if the condition lasts very long although it may reduce in size when the androgen use is discontinued. In the absence of resolution, surgical correction may be necessary in severe cases.
For men who experience enlarged breast size, doctors usually check estradiol levels to determine whether too much testosterone is being converted into estrogen. I do not believe that routine measurement of estrogen is needed for men who have no symptoms of high estrogen (mainly breast tissue enlargement and water retention). For those who have higher than normal estrogen, doctors usually prescribe an antiestrogen medication. One such regimen is anastrozole at 1 mg/day during the first week until nipple soreness and breast enlargement disappear. The dose is then lowered to 0.25 mg a day, or 1 mg twice a week.
A warning: Bringing estrogen down to very low levels could cause health problems in men in the long run. Hair/skin quality and health, brain function, bone density, and other important factors may be greatly influenced by estrogen. However a 12-week study in men using anastrozole at 1 mg a day and 1 mg twice a week found no changes in bone metabolism markers.
The normal production ratio of testosterone to estrogen is approximately 100:1. The normal ratio of testosterone to estrogen in the circulation is approximately 300:1. Estrogen (measured as estradiol) should be kept at 30 picograms per milliliter (pg/mL) or lower. As men grow older or as they gain a lot of fat mass, their estrogen blood levels increase, even to levels higher than that of postmenopausal women.
Medications and Products That Can Cause Gynecomastia
A number of medications have been reported in the medical literature to cause gynecomastia due to decreases in testosterone, increases in estradiol, or both. These include:
- Antiandrogens. These include cyproterone, flutamide, and finasteride.used to treat prostate cancer and some other conditions.
- HIV medications. Sustiva, Atripla, and Videx have been associated with gynecomastia.
- Anti-anxiety medications such as diazepam (Valium).
- Tricyclic antidepressants. These include amitriptyline.
- Glucocorticoid steroids.
- Antibiotics.
- Ulcer medication such as cimetidine (Tagamet).
- Cancer treatment (chemotherapy).
- Heart medications such as digitalis and calcium channel blockers.
- Anabolic steroids
Substances that have been reported to cause gynecomastia include:
- Alcohol
- Amphetamines
- Marijuana
- Heroin
- Soy and flaxseed – There are conflicting studies but it is something to keep in mind
- Exposure to pesticides and byproducts of plastic processing has also been linked to increased estrogen and decreased sperm count in men.
Does Testosterone Suppress the Immune System?
This question is raised out of the confusion over the use of the term “steroid.” When somebody is having pain or inflammation and their physician prescribes them a “steroid” or something “steroidal”, they are prescribing a corticosteroid (like prednisone) to decrease inflammation. These can have an immunosuppressive effect (sometimes its intended). The “steroid” that you hear about from the media when they are talking about use and abuse by athletes refers to an anabolic steroid (like testosterone). The similarities largely end with their street names.
Some in vitro and animal data do suggest that high dose testosterone could be immune suppressive. No such immunosuppressive effect is seen when testosterone was added at replacement concentrations. Several studies using testosterone alone or on combination with oxandrolone or nandrolone in HIV-positive immune compromised patients have found no immune suppressive effect.
Excerpted from “Testosterone: A Man’s Guide“.
About the author
Nelson Vergel is the author of "Testosterone: A Man's Guide- Second Edition" and co-author of the book "Built to Survive: A Comprehensive Guide to the Medical Use of Anabolic Therapies, Nutrition and Exercise for HIV (+) men and women", the founder of the Body Positive Wellness Clinic in Houston, and an expert speaker on exercise, nutrition, testosterone replacement, metabolism , sexual function and therapies to increase lean body mass and decrease fat.
Thank you for this article, this is exactly what I have been looking for. I have been on TRT for 3 years and my test level is at 315, the Doctor is fine with this level but I am not, I want to use this article and the information contained within to convince the DR. to increase the amount of Test that I am taking. So again thank you.