July 9, 2002 marked an historic date in medical history. In one of the biggest scandals in medical history, government scientists shut down a study on the most commonly used hormone replacement therapy used in the country. These researchers concluded that it was no longer ethical to keep administering the infamous Prempro hormone replacement drug combination to post-menopausal women in a multi-center research study because it was inflicting more harm than good.
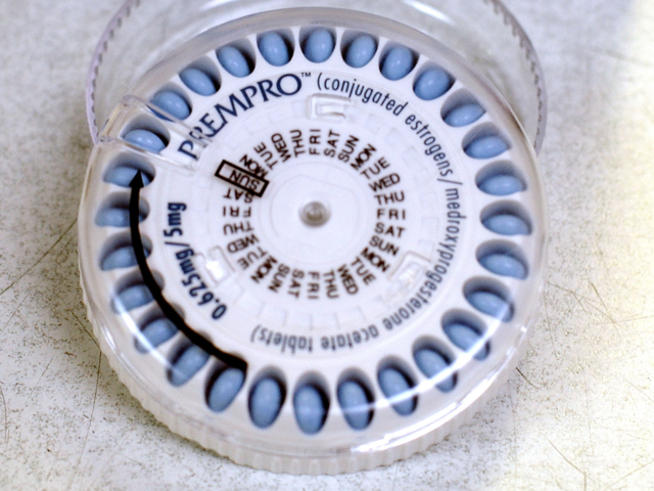
This was an indeed an historic and scandalous event. Millions and millions of women have been placed on this combination of Premarin and Provera (Prempro), which are synthetic versions of the hormones estrogen (CEE: conjugated equine-horse estrogens) and progesterone (MPA: medroxyprogesterone acetate). Premarin has been around since 1942, and is one of the most widely prescribed drugs in history. It was the single most prescribed drug every year between 1992 and 1999 (1). Women were lead to believe that they would live longer and healthier lives if they would take Premarin or Prempro. Doctors believed all the propaganda fed to them by the makers of these drugs. But the recent decision by the National Heart, Lung, and Blood Institute (NHLBI) and the Women’s Health Initiative (WHI) to discontinue this study supports what I have been saying for many years, that Premarin and Provera are toxic and do more harm than good.
However, I am concerned that the media will misinterpret the results of this study. Unfortunately, hormone replacement therapy is getting a bad name. While I have been an opponent of the Premarin and Provera strategy for a long time, there are safe and effective alternative hormone replacement therapy programs that I have been using successfully in my private practice for a long time. My own approach emphasizes natural, human bio-identical hormones rather than toxic and synthetic drugs such as Premarin and Prempro. In this article, I want to go over what the key implications of the NHLBI/WHI study are, and give some guidelines for doctors and post-menopausal women who are still interested in an alternative approach to hormone replacement therapy.
Background
How could it happen, that millions of women could be given a toxic drug combination for so long? Part of the reason is that faulty research was used to promote these drugs. Initial studies showed that Premarin or Prempro could decrease the risk of heart disease. However, these studies were fatally flawed. The main problem with these studies is that they were observational rather than long term prospective controlled studies. This means that researchers went out and found women who had already made their own personal decision to go on Premarin or Prempro. It was found that these women on average had less risk of heart disease than women who had not chosen to take Premarin or Prempro.
However, this approach is biased in favor of these drugs. You see, women who decided to take these drugs were usually more health conscious than the average woman. They tended to eat healthier foods and exercise more than women who did not take Premarin or Prempro. Thus these women had less risk of heart disease in spite of the drugs they took, not because of them. Healthy lifestyle choices counterbalanced the negative effects of Premarin and Prempro. But the negative effects of these drugs would not be completely exposed until the results of the NIH study were recently announced.
The NHLBI Study
The results of this groundbreaking study on Prempro were published in the July 17 issue of the Journal of the American Medical Association (JAMA) (2). I found this study to be a very impressive, with a large sample population and excellent research methods. This study used 16,608 post-menopausal women, with an age range of 50-79 years old. These women were randomly given either the Prempro synthetic estrogen and progestin combination, or a placebo. The fact that this study was a randomized, placebo controlled study is highly significant. As mentioned before, much of the previous research on Prempro was not randomized or placebo controlled, and thus suffered from sample bias. The randomized, placebo controlled nature of this study means that most possible sample biases were eliminated from the study.
In addition to having a large sample population with a randomized, placebo controlled methodology, this study also looked at this women for a long time period. Women in this study were looked at for an average of 5.2 years. Thus I find the results of this study highly conclusive and most compelling.
The main results of this study were quite shocking to the medical community, although I was not surprised at all. Prempro was found to increase the risk of breast cancer, heart disease, strokes, and blood clots. The fact that Prempro increased the risk of heart disease was especially shocking, since one of the main reasons hormone replacement therapy is often prescribed is to fight heart disease. But it turns out that Prempro will actually increase your risk of heart disease.
The only real positive effects of Prempro were to decrease the risk of hip fractures and colon cancer. But these were more than cancelled out by the increase risk of heart disease and other risks mentioned above.
Implications
The first and most obvious implication of this study is to stop using Prempro immediately! I am troubled by a recent poll showing many doctors do not plan to stop prescribing Prempro in spite of the results of this study (3). Part of the Hippocratic oath all medicals doctors take before they start practicing medicine is “do no harm”. Prescribing Prempro is clearly a violation of this oath.
I believe that of the two drugs that make up Prempro, the Provera (postent synthetic progesterone) portion is responsible for a majority of the negative effects found with Prempro. Not only should doctors stop prescribing Provera, but I also believe that the FDA should consider removal of its approval of this toxic drug and remove it from the market.
Some doctors and scientists have pointed out that the risks found in this study were relatively small. However, the average length of time women were on Prempro in this study was 5.2 years. These risks could increase exponentially if you were to take Prempro for 10, 20, or more years. Also, this study did not look at effects of Prempro on body composition. I have noticed in my private practice that Premarin promotes bloating and fat storage, whereas as Provera increases appetite and decreases energy and motivation. Obesity is probably another significant risk of Prempro that should be explored further (for more on the effects of hormones on your body composition, see my forthcoming book The Hormone Revolution Weight Loss Plan, Avery Press/Penguin-Putnam).
While this study was highly conclusive in showing negative effects for Prempro, it is limited in that only applies to the specific drugs that make up Prempro – Premarin and Provera. The authors of this study point out that “It remains possible that transdermal estradiol with progesterone, which more closely mimics the normal physiology and metabolism of endogenous sex hormones, may provide a different risk-benefit profile.” I find this statement interesting, since this approach mentioned by the doctors is quite similar to my own hormone replacement protocol for women.
My Own Hormone Replacement Therapy Protocol
I have spent many years carefully developing my own alternative approach to hormone replacement therapy. I hope more and more doctors and patients will pay more attention to my protocol in light of the results of the recent Prempro study. My approach is to take a case by case approach to the use of all three major sex hormones: estrogen, testosterone, and progesterone in their natural, human bio-identical forms.
Estrogen:Since even natural estrogen can increase the risk of breast cancer and promote fat storage and weight gain, I take a very cautious approach to the use of estrogen in an overall hormone replacement program.
One of the most common reasons why post-menopausal women request estrogen replacement therapy is because of hot flashes. Estrogen is indeed very potent most of the time at preventing hot flashes, sweating, and other heat regulation problems associated with menopause. But it is not necessary to immediately start with estrogen at the first sign of hot flashes, as there are other options. The safest way to fight hot flashes without side effects is to eat a diet high in natural plant estrogens (phytoestrogens). Good food sources of phytoestrogens include soy products, chick peas, lentils, flax seeds, and various other legumes and nuts. If you do not get enough phytoestrogens from your diet, another option for women is try to treat their hot flashes with phytoestrogen supplements such as black cohosh, red clover, or soy. For many women, a safe and natural phytoestrogen supplement or high-phytoestrogen diet will do the trick. This is preferable, since phytoestrogens usually do not cause you to get fatter and do not increase the risk of breast cancer.
For women who still get hot flashes in spite of a high phytoestrogen diet and/or use of phytoestrogen supplements, stronger therapy might be necessary. In these cases, I recommend low doses of natural, human bioidentical estrogens. These are much safer and have few side effects than the horse estrogens found in Premarin. I also prefer transdermal patches or creams instead of oral pills. One study showed that oral Premarin lead to fat gain and less of the growth factor hormone IGF-1, while transdermal human bioidentical estrogen did not have these negative side effects (4). But even with these natural transdermal estrogens, I only recommend t he minimum possible dose that will effectively treat hot flashes, insomnia, and other common symptoms of menopause.
For women who wish to take estrogen solely to decrease their risk of breast cancer, I discourage them from doing this until they are at least the age of 60. I don’t think it is necessary to go as far as taking estrogen to fight heart disease when they are many other options, such as improving your diet, starting an exercise program, taking statin drugs, taking fish oil supplements, and many other options. Heart disease is really only a risk later in life, but breast cancer is a risk for women at almost any age. Therefore, I think taking estrogen as a way to fight heart disease should be delayed as long as possible to avoid increasing the risk of breast cancer and all the other problems associated with estrogen use.
Estrogen can help delay osteoporosis, but should be considered only one part of an overall prevention program. Women at risk for osteoporosis should be taking 1,200 t0 1,500 milligrams of calcium plus 800 to 1000 i.u. vitamin D every day, and should also be on a regular weight training program. When you weight train the strain you put on the bones/muscle signals bones to get stronger. There are also non-hormonal drugs that help build up bone and decrease osteoporosis and fracture risk without the side effects associated with estrogen.
Testosterone:This hormone is almost completely overlooked when hormone replacement therapy is prescribed for women. But in my experience I have found testosterone to have the much greater effects in post-menopausal women than any estrogen or progesterone treatment. Ever since I wrote the first “Testosterone for Women” article for this magazine, I have been flooded with email from women. Testosterone, when used appropriately, can dramatically increase libido, improve mood, increase energy and fight fatigue, and lead to increased fat loss. Testosterone may even lead to lower breast density which leads to a lower risk of breast cancer.
Like my approach with estrogen, I only recommend natural, human bioidentical testosterone for use in a hormone replacement program. The problem is that there are not many testosterone products available for women. One of the few testosterone drugs manufactured for women is Estratest. Unfortunately, this drug contains synthetic methyltestosterone, which can be liver toxic at high doses and also can lower good HDL cholesterol levels.
One commonly available options to increase a women’s testosterone levels is the natural hormone supplement DHEA. DHEA (dehydroepiandrosterone) is a naturally occurring hormone that converts to testosterone in two steps in the body. DHEA is cheap and widely available at any vitamin store or health food store. While DHEA is largely ineffective in men (often boosting estrogen more than testosterone), it is highly effective at boosting testosterone in women. DHEA may also have other benefits other than boosting testosterone, such as an improved immune system. The typical dose of DHEA I recommend for women is in the range of 5 to 25 milligrams, starting at the lower end and building up until the desired effect is reached.
Another option for women is the prohormone supplement that is sold under than brand name Androdiol (scientific name 4-androstenediol). This supplement is relative safe in that it only causes a brief and temporary spike in testosterone levels. Women can safely use this supplement if they want a little boost before or during sex or exercise. Unfortunately, it is difficult to find Androdiol in doses appropriate for a women. Most Androdiol supplements come in male doses of 100 to 200 milligrams, far more than the 5 to 25 milligram dose appropriate for women. There are only a few powder and liquid Androdiol products that allow you to adjust the dose to a low enough level.
Finally, you can also have your MD prescribe from compounding pharmacy a transdermal testosterone cream or gel. These transdermal testosterone products are useful for promoting an even, steady release of testosterone into the blood stream. Like with DHEA and Androdiol, I also recommend a “start low and go slow approach”. Testosterone is extremely potent in women, and a cautious approach is the best.
For women on some form of estrogen, I almost always recommend the addition of testosterone to their hormone replacement program. Testosterone and estrogen exist in the human body in a natural “yin-yang” fashion as they tend to balance each other out. I believe that including testosterone along with estrogen will counter some of the possible negative side effects of estrogen, such as bloating and fat/weight gain. Testosterone also will help estrogen in building up bone mass and fighting osteoporosis.
Progesterone: I have found that natural, human bioidentical progesterone has radically different effects on women than the toxic and synthetic Provera. While Provera sometimes causes women to become aggressive and agitated, natural progesterone has a calming and relaxing effect. Like with estrogen and testosterone, I also recommend progesterone to be used as a transdermal cream or gel. I recommend that it be applied to the anterior neck at night time to induce better sleep and tranquilty. Natural progesterone can help reduce the risk of endometrial cancer, and unlike Provera will not increase the risk of heart disease. If you are going to use a progesterone, make it natural progesterone.
| Hormone | Standard Medical HRT Protocol | Dr. Ullis HRT Protocol |
| Estrogen | Synthetic horse estrogen pills (Premarin) | Natural plant phytoestrogens,Natural human bio-identical estrogen gel or cream |
| Progesterone | Synthetic Provera | Natural progesterone |
| Testosterone | None | DHEA,Natural testosterone gel or cream |
Conclusion
The NHBLI/WHI study is truly grounding breaking, and will forever change the medical community’s view of hormone replacement therapy. I am happy that the Premarin/Provera combination has finally been conclusively discredited. However, I am concerned that the baby will be thrown out with the bath water. When hormone replacement therapy is done correctly, it can dramatically improve your life for the better and increase your lifespan and quality of life.
But remember, hormone replacement therapy is just one part of an overall anti-aging lifestyle program. If you eat unhealthy foods and do not exercise correctly, no form of hormone replacement therapy will help you stay young. But cautious, careful use of natural, human bio-identical hormones can definitely give your anti-aging program the “extra edge” for a long and youthful lifespan.

About the Authors
Karlis Ullis, M.D., is a board-certified physician and an assistant clinical professor at the UCLA School of Medicine. He has worked with intercollegiate, professional, and Olympic athletes and served as team physician in five Olympic games. He practices in Santa Monica, California, and is the author of Age Right and Super “T”. His next book will be The Hormone Revolution Weight Loss Plan (Avery Press), which will be released January 30, 2003.
Joshua Shackman, Ph.D.., is an assistant professor of Management and Health Sciences at Touro University International. He lives in Los Angeles.
References
(1) Mercola, Joseph “Bombshell: Major Premarin Trial Halted” eHealthy News you can Use. http://www.mercola.com/2002/jul/13/index.htm
(2) Rossouw, Jacques E. et al., “Risks and Benefits of Estrogen Plus Progestin in Healthy Postmenopausal Women” JAMA, July 17, 2002
(3) Peterson, Melody, “Survey Halted, Drug Makers Seek to Protect Hormone Sales” New York Times, July 17, 2002
(4) O’Sullivan AJ, Crampton LJ, Freund J, Ho KK. “The route of estrogen replacement therapy confers divergent effects on substrate oxidation and body composition in postmenopausal women.” J Clin Invest. 1998 Sep 1;102(5):1035-40.
About the author
Warning: Undefined array key "display_name" in /home/thinksteroids/public_html/wp-content/plugins/molongui-authorship-pro/includes/hooks/author/box/data.php on line 11
Warning: Undefined array key "display_name" in /home/thinksteroids/public_html/wp-content/plugins/molongui-authorship-pro/includes/hooks/author/box/data.php on line 11
Warning: Undefined variable $show_related in /home/thinksteroids/public_html/wp-content/plugins/molongui-authorship/views/author-box/parts/html-tabs.php on line 30


Leave a Reply
You must be logged in to post a comment.