Prostate Specific Antigen (PSA), TRT, and Finasteride
Q: I have watched my PSA rise and have had some urological problems recently. I have seen 3 urologists. One said discontinue TRT now and the other two were not quick to discontinue anything. Should older guys be thinking about a 5AR while on exo test?
A: Brief discussion below. Also, have you considered the use of finasteride, etc.? A thought after any pathology has been ruled out.
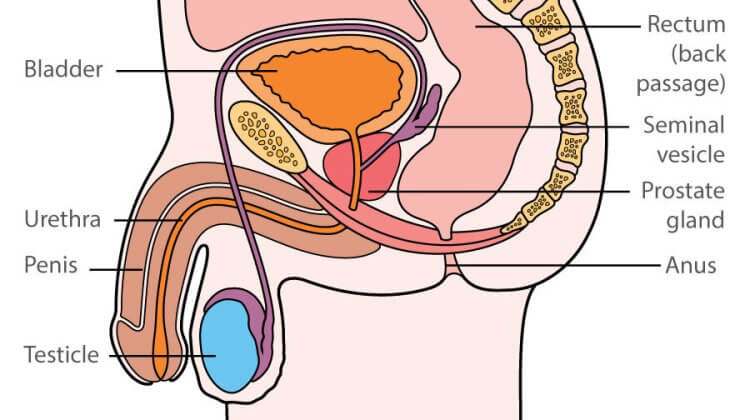
Benign Prostatic Hyperplasia – The development of BPH requires the presence of androgens and that the marked reduction in serum testosterone caused by chemical or surgical castration causes reduced prostate volume. Studies have failed to demonstrate exacerbation of voiding symptoms attributable to BPH during testosterone supplementation.
Prostate volume, as determined by ultrasonography, does increase significantly during testosterone-replacement therapy.Urine flow rates, postvoiding residual urine volumes, and prostate voiding symptoms did not change significantly in these studies. This is explained by the poor correlation between prostate volume and urinary symptoms. Individual men with hypogonadism may occasionally have increased voiding symptoms with TRT.
Prostate Cancer – There is no scientific peer-reviewed literature that definitely establishes a link between the administration of testosterone and the increasing the risk or development of prostate cancer. There is no compelling evidence that testosterone has a causative role in prostate cancer or to suggest men with higher testosterone levels are at greater risk of prostate cancer or that treating hypogonadism with exogenous androgens increases this risk. Just remember the incidence of prostate cancer rises with aging which is associated with declining testosterone levels. Prostate cancer becomes more prevalent exactly at the time of a man’s life when testosterone levels decline.
Over 200,000 men are given a diagnosis of prostate cancer each year and most are first detected by a rise in the PSA level unrelated to testosterone therapy.
Interestingly the underlying prevalence of occult prostate cancer in men with low testosterone levels appears to be substantial. A history of prostate cancer has been considered an absolute contraindication to testosterone-replacement therapy which is now under active debate for men who are deemed cured.
PSA – The 2002 U.S. Preventative Services Task Force recommendations on the screening for prostatic cancer concludes that the evidence is insufficient to recommend for or against routine screening for prostate cancer using prostate-specific androgens (PSA) testing or digital rectal examination (DRE), “Screening is associated with important harms including frequent false-positive results and unnecessary anxiety, biopsies, and potential complications of treatment of some cases of cancer that have never affected a patient’s health. The USPSTF concludes that evidence is insufficient to determine whether the benefits outweigh the harms for a screened population.”
PSA values used to trigger prostate biopsy include an increase of 1.5 ng per milliliter within two years or a total increase of 2.0 ng per milliliter over any period. These recommendations have been based on observational population studies in untreated men. I would use 0.75 ng over 12 months.
These are free downloadable files.
Rhoden EL, Morgentaler A., Risks of testosterone-replacement therapy and recommendations for monitoring, N Engl J Med. 2004 Jan 29;350(5):482-92.
Screening for prostate cancer: recommendation and rationale. (2002). Ann Intern Med, 137(11), 915-916.
Recommendations if PSA is high BUT Prostate Biopsy is Negative
Q: if a man tests high on a single PSA or shows some acceleration in PSA with numbers as you suggest AND evaluation by biopsy proves negative, should continued high scores on PSA be ignored? Should avadart or something similar be used to lower the score?
A: I had a number of patients with an elevated PSA. Each was checked out by a urologist with periodic monitoring. The acceleration is something I would particularly careful for. It is pretty unusual to have sexual dysfunction while on T and an alpha –reductase blocker. I usually suggested to patients. One could use Dutasteride (forgot the brand name) instead of Finasteride but it is probably not worth the cost. Overall, dutasteride is a more efficient steroid 5 -reductase inhibitor than finasteride. They have been shown to be protective for prostate cancer. But, as I said previously there are no studies linking TRT to PrCa. Testosterone replacement therapy in men with erectile dysfunction and hypogonadism is associated with a minor PSA elevation.
In a study in hypogonadal men with and without high grade prostatic intraepithelial neoplasia (PIN), which is considered a prostatic precancerous lesion, after 1 year of TRT men with PIN did not have a greater increase in PSA or a significantly increased risk of cancer than men without PIN. These results indicate that TRT is not contraindicated in men with a history of PIN.
Dihydrotestosterone (DHT) is the primary metabolite of testosterone in the prostate and skin. Testosterone is converted to DHT by 5alpha-reductase, which exists in two iso-enzyme forms (types 1 and 2). DHTis associated with development of benign prostatic hyperplasia (BPH), and reduction in its level with 5 alpha-reductase inhibitors improves the symptoms associated with BPH and reduces the risk of acute urinary retention and prostate surgery. A selective inhibitor of the type 2 iso-enzyme (finasteride) has been shown to decrease serum DHT by about 70%.
We hypothesized that inhibition of both iso-enzymes with the dual inhibitor Dutasteride would more effectively suppress serum DHT levels than selective inhibition of only the type 2 iso-enzyme.
DIHYDROTESTOSTERONE (DHT), A STEROID hormone produced from testosterone by the enzyme 5alpha- reductase is the primary active metabolite of testosterone. In male fetal development and puberty, it is essential for normal masculinization of the external genitalia and normal development of the prostate gland. In later life, DHT is associated with the development of benign prostatic hyperplasia (BPH) and androgenetic alopecia. The enzyme 5 alpha-reductase is present throughout the body in two forms, type 1 and type 2. Type 1 has been reported to be located predominantly in the skin, both in hair follicles and sebaceous glands, as well as in the liver, prostate, and kidney. Type 2 is found in the male genitalia and the prostate; recent research has also identified type 1 mRNA and enzyme activity in the prostate.
The first available 5-alpha reductase inhibitor (finasteride) is selective for the type 2 iso-enzyme. Its clinical utility in reducing enlarged prostates, relieving symptoms associated with BPH, and reducing the risk of associated complications has been documented in several clinical trials. More recently, 5 alpha-reductase inhibition has been proven effective in treating androgenetic alopecia. Finasteride suppresses serum DHT by about 70%. Dutasteride is a 6-azasteroid, which inhibits both type 1 and type 2 5_-reductase iso-enzymes. The IC50 for type 1 5 alpha-reductase is 0.7 and 81.0 nm for dutasteride and finasteride, respectively, and for type 2 5 alpha-reductase, 0.05 and 0.16 nm, respectively.
New Markers for Prostate Cancer
Q: have you used the AMACR in lieu of the PSA? Is AMACR ready to replace PSA as a PC indicator?
A: I have no personal experience with AMCAR. I do not think it is even commercially available. For others a brief background follows with some links to downloadable articles.
Prostate specific antigen (PSA) is a sensitive serum marker for pathology in the prostate (cancer, infection, benign hyperplasia). The level of PSA, however, is poorly correlated with grade and stage of prostate cancer. Genomic and proteomic methodology has recently been used to discover more then 200 putative new markers for prostate cancer like alpha-methylacyl CoA racemase (AMACR), hepsin, glutathione S-transferase ?, EZH2 and DD3(PCA3). To date, none of these markers have been adequately validated for clinical use.
Prostate cancer is the second-leading cause of cancer-related death in American men (1). Although the use of prostate-specific antigen (PSA) screening has led to the earlier detection of prostate cancer, the impact of PSA screening on cancer-specific mortality is still unknown, pending the results of prospective randomized screening trials. Interpretation of the serum PSA test is made on the basis of PSA levels, with levels of 0–4 ng/mL being considered normal and levels of greater than 4 ng/mL being considered clinically significant for prostate cancer screening. A major limitation of the serum PSA test is its lack of specificity for prostate cancer, especially in the intermediate range of PSA levels (4–10 ng/mL). In this range, the specificity of the PSA test to detect prostate cancer has been reported to be only 20% at a sensitivity of 80%. This poor specificity is, in part, associated with the fact that serum PSA levels can be increased in patients with nonmalignant conditions such as benign prostatic hyperplasia or prostatitis and that PSA is highly expressed in both benign prostatic epithelia and prostate cancer cells.
One such prostate cancer biomarker is -methylacyl-CoA racemase (AMACR), an enzyme that catalyzes the racemization of R-stereoisomers of branched-chain fatty acids to S-stereoisomers and plays an important role in peroxisomal -oxidation of branched-chain fatty acids. Differential display and expression array analyses have identified the AMACR gene as a gene whose expression is higher specifically in prostate cancer epithelia relative to benign prostatic epithelia. AMACR is a highly specific and sensitive marker for cancer cells within the prostate gland. In addition, a recent study demonstrated that sequence variants of AMACR may be associated with prostate cancer risk. Although AMACR may be potentially useful in the diagnosis of prostate cancer from tissue specimens, it would have considerably more utility as a tumor marker if it could be detected in serum.
http://jncicancerspectrum.oxfordjournals.org/cgi/content/full/jnci;96/11/834
http://ajp.amjpathol.org/cgi/content/full/164/3/831
About the author
The research of Michael Scally focuses on returning individuals to normal physiology after the discontinuation of anabolic steroids. Dr. Scally has presented his medical protocol for the treatment of Anabolic Steroid Induced Hypogonadism before the Endocrine Society, American Association of Clinical Endocrinologists, American College of Sports Medicine, and International Workshop on Adverse Drug Reactions and Lipodystrophy in HIV. Dr. Scally is the author of "Anabolic Steroids - A Question of Muscle: Human Subject Abuses in Anabolic Steroid Research."
Leave a Reply
You must be logged in to post a comment.