My Current Best Thoughts on How to Administer Testosterone Replacement Therapy (TRT) for Men
We have already learned a practical bit about the various hormones that make up the metabolic “symphony” which comprises our hormonal milieu. We know where these hormones are produced, what modulates their production, and the target tissues of their various and varied actions. But we still need to integrate this knowledge into a practical “recipe”, if you will, so the clinician may return to his/her practice, and immediately begin screening for, and successfully treating, male hypogonadism. In other words, how do you actually administer Testosterone Replacement Therapy for men?
Should EVERY adult male patient who presents at your office be automatically screened for hypogonadism? About half of all men over the age of fifty are in fact hypogonadal (when tested for Bioavailable testosterone—more on that later). Certainly the answers to Medical History will lead the way toward suspicion of same, yet the complaints related to this insidious condition are sensitive without being specific. Clinical suspicion is further clouded because there is no way to correlate either the number of individual complaints, or the relative magnitude of each, to the severity of the hypogonadotrophic state on laboratory assay. The number one complaint which should hoist the proverbial red flag is Erectile Dysfunction. This is also the symptom of hypogonadism which, aside from all the seriously deleterious effects of same (coronary artery disease, diabetes, osteoporosis, increased risk of cancer, depression, dementia, etc.), is most likely to bring the patient to actively seek TRT—and to remain compliant in your treatment regimen.
INITIAL LABWORK
Following a good Medical History, which laboratory assays should be run as part of your initial hypogonadism workup? Following is my list, but certainly other specialists in this area run expanded or attenuated panels, per their experience and expertise. Of note, there are several other tests which should be included to complete the true comprehensive Anti-Aging Medicine workup (i.e. homocysteine, fasting insulin, comprehensive thyroid study, etc.), as this chapter is concerned solely with administering TRT. And as always, the panel is tailored to the individual patient. Here they are:
- Total Testosterone
- Bioavailable Testosterone (AKA “Free and Loosely Bound”)
- Free Testosterone (if Bioavailable T is unavailable)
- DHT
- Estradiol (specify the Extraction Method, or “sensitive” assay for males)
- LH
- FSH
- Prolactin
- Cortisol
- Thyroid Panel
- CBC
- Comprehensive Metabolic Panel
- Lipid Profile
- PSA (if over 40)
- IGF-1 (if HGH therapy is being considered)
FOLLOW-UP LABS
Two weeks after initiating a transdermal, or five weeks after the first IM injection:
- Total Testosterone
- Bioavailable Testosterone
- Free Testosterone (if Bioavailable T is still unavailable)
- Estradiol (specify the Extraction Method, or “sensitive” assay for males)
- DHT (especially if patient is using a transdermal delivery system)
- FSH (3rd Generation—ultrasensitive assay this time)
- CBC
- Comprehensive Metabolic Panel
- Lipid Profile
- PSA (for more senior patients)
- IGF-1 (if GH Therapy has been initiated already)
INDIVIDUAL ASSAYS EXPLAINED
TOTAL TESTOSTERONE
This is the assay your patients will most focus on. It’s also the one physicians who do not understand TRT will use to deny patients the testosterone supplementation they want, and need, when Total T is at low-normal levels. Total T is important for titration of dosing, but its relevance is reduced in older men (by virtue of their increased serum concentrations of SHBG), in favor of:
BIOAVAILABLE TESTOSTERONE
Where we actually get the “bang” for the hormonal buck, so to speak. This is the actual amount the body has available for use, as the concentration of hormone available within the capillary beds approximates the sum of the Free Testosterone plus that which is loosely bound to carrier proteins, primarily albumin. If Bio T is not readily available, Free T may be a second choice substitute, as Bio T and Free T serum concentrations are well correlated.
DHT
This assay is especially important to draw, up-front and at follow-up, if a transdermal testosterone delivery system is preferred by the patient. I’ll explain why later. DHT level may also help indicate cause for ED symptoms.
ESTRADIOL
There are several reasons why this assay is VERY important, and should not be ignored in ANY hypogonadism work-up (or subsequent regimen). First, you definitely need to draw a baseline. Next, elevated estrogen can, in and of itself, explain hypogonadal symptoms. If E is elevated, controlling serum concentrations (usually with an aromatase inhibitor, which prevents conversion of T into E) may suffice in clearing the symptoms of hypogonadism. And finally, rechecking it after beginning the initial dose of testosterone will give the astute physician valuable information as to how the patient’s individual hormonal system functions, as well as making sure estrogen does not elevate inappropriately secondary to the testosterone supplementation.
I don’t waste time and money drawing estrone and estriol. E2 is the player of interest here. Unless you specify a ‘sensitive’ assay for male patients, the lab will run the Rapid Estradiol for fertility studies in females, which is useless for our purpose here. Quest Diagnostics calls this their Estradiol by Extraction Method.
Some practitioners believe that it is only the T/E ratio which is significant, and therefore, as long as E “appropriately” rises with elevations in T, all is well. However, the absolute concentration of E is of concern, too, especially in light of new information pointing to elevated estrogen as cause, or adjunctively encouraging, several serious disease processes, including prostate and colon cancer.
LH
As everyone knows, it is LH which stimulates the Leydig cells of the testes to produce testosterone. A caveat, however: LH has a half-life of only about 30 minutes. When you combine this fact with the absolute pulsatile nature of its pituitary release, care must be taken to not place too much weight upon a single draw. A luxury would be to acquire serial draws, say, twenty minutes apart. However, such would be both inconvenient and probably prohibitively expensive for the patient. The most important reason to assay the gonadotrophins is to differentiate between primary and secondary (hypogonadotrophic) hypogonadism.
FSH
The eight hour half-life of this hormone makes it a better marker for gonadotrophin production. It is also less an acute phase reactant to varying serum androgen and estrogen levels than LH. Greatly elevated FSH levels could signal a gonadotrophin-secreting pituitary tumor.
Of note, I run FSH (but not LH) on the follow-up labs, the new third generation (“sensitive”) assay, to determine the magnitude of HPTA suppression secondary to androgen therapy. It also provides valuable information for those patients undergoing TRT who are interested in the state of their fertility.
PROLACTIN
A very important hormone, and must not be overlooked on initial work-up. Approaching five percent of hypogonadotrophic hypogonadism is associated with hyperprolactinemia, due to inhibition of hypothalamic release of LHRH. Its serum concentration must be maintained within physiological range (meaning neither too high nor too low). Greatly elevated hyperprolactinemia, or hyperprolactinemia plus a Total Testosterone less than 150ng/dL, equals a trip to an Endocrinologist for an MRI of the sella turcica.
CORTISOL
True Anti-Aging medicine must be well-familiarized with the ins and outs of this hormone, the only one our bodies cannot live without. Elevated levels can cause secondary (hypogonadotrophic) hypogonadism. I try controlling elevated cortisol with Phosphatidylserine, 300mg QD, with good results. It is just as important to watch for depressed cortisol levels, as well. The assay of choice for that condition is a 24-hour urine.
THYROID PANEL
I have, for my own convenience, omitted the specifics of the obligatory thyroid function panel you certainly will want to run. Hypothyroidism mimics hypogonadism in several of its effects.
CBC
This is just good medicine. Ruling out anemia is important, of course, as it may be a cause for the fatigue which brought the patient into your office. You also want to establish baseline H&H, for those rare cases where polycythemia becomes a problem (and we are reminded smokers are at increased risk for polycythemia). Above 18.0/55.0 TRT is withheld, and therapeutic phlebotomy recommended.
CMP
Again, just good medicine. Baseline for sodium (which may elevate initially secondary to androgen supplementation) is important. We also want to see LFT’s, as elevations in same secondary to androgen supplementation are listed as a possible side effect in the product literature (although I have yet to see this actually happen). I like the BUN/creatinine ratio as a marker for hormonal hemo-concentration, and also it gives me a hint of how compliant the patient will be (because I always tell them to make sure to drink plenty of water while fasting for the test).
Lipid Panel
This is drawn to provide your bragging rights when you drop the CHOL 30 points, thanks to your own good administration of TRT. You should expect to see lowered TRIG and LDL’s, too. Be advised, this will not happen if you choose to elevate their androgens above the top of “normal” range, i.e. providing what amounts to an anabolic steroid cycle. Of course, this would no longer constitute TRT, as the practitioner would then be choosing to damage the health and well-being of the patient.
HDL does frequently drop a bit, but that is believed to be due to increased REVERSE cholesterol transport; so much of the plaque is, after being scavenged from the lining of the CV system by HDL, now being chewed up by the liver. Androgens also elevate hepatic lipase, and this may have an effect. The important thing to keep in mind is that TRT inhibits foam cell formation.
PSA
For all patients over 40. Even though prostate CA is rare in men under the age of fifty, we don’t want it happening on our watch, do we? At this time, rises in PSA above 0.75 are a contraindication to TRT (until follow-up by a Urologist). You may find that, at the initiation of TRT in older men, when serum androgen levels are accelerating, PSA may, too. This is especially true when transdermal delivery systems are employed, because they more greatly elevate DHT. Once T levels have stabilized, PSA drops back down to roughly baseline. You won’t really see gross elevations in PSA secondary to TRT administration in younger patients. New TRT patients need to be cautioned, and reminded, to abstain from sexual relations prior to the draw, as they may now be enjoying greatly elevated amounts of same.
I get a PSA up front on my over 40 patients, at the one month follow-up in my more senior patients, and every six months after that. DRE (Digital Rectal Exam) is recommended twice per year as well, although the American Academy of Clinical Endocrinologists backs “every six to twelve months” in their 2002 Guidelines for treating hypogonadotrophic patients with TRT.
IGF-1
For those who are considering the addition of GH to their Anti-Aging regimen. IGF-1 will rise from testosterone supplementation, and vice versa. Let’s grab a baseline now, before that happens.
THINGS TO LOOK OUT FOR
CO-MORBIDITIES. Currently, only breast and active prostate cancer are absolute contraindications for TRT. Patients with serious cardiac, hepatic or renal disease must be monitored carefully due to possible edema secondary to sodium retention. Also, TRT may potentiate sleep apnea in some chronic pulmonary disease patients, although studies have also shown it can actually ameliorate the symptoms of sleep apnea.
DRUG INTERACTIONS. TRT decreases insulin or oral diabetic medication requirements in diabetic patients. It also increases clearance of propranolol, and decreases clearance of oxyphenbutazone in those receiving such medications. TRT may increase coagulation times as well.
TESTOSTERONE DELIVERY SYSTEMS
Now we have to decide, TOGETHER with our patient, what form of testosterone delivery system we will START with. There are two basic subsets of same—transdermals and injectables. Here are the current options:
TESTOSTERONE GELS AND CREAMS
The only way to go, in my professional opinion, if physician and patient prefer a transdermal delivery system. They are easy to apply, well absorbed, and rapidly establish stable serum androgen levels (usually by the end of the second day).I recommend all practitioners first try a testosterone gel for their TRT patients.
Much is made of the risk posed by accidental transferal of testosterone to others, such as children or sexual partners. Simply covering with a T-shirt has been shown to block transfer of the hormone. The testosterone sinks into the skin within an hour, which acts as the actual reservoir for the hormone’s delivery. One may then shower, or even swim, without worry. I remind my patients that most of us have neither the time, nor the opportunity, for romance until evening (given the recommended early morning application), and a quick shower is always nice to “freshen up” then anyway.
Gels and creams, like all transdermal delivery systems, provide a bigger boost in DHT levels, compared to injectable testosterone preparations. This can be a double-edged sword. As DHT is responsible for all the things of manhood, the transdermals are better at treating ED than the injectables. However, issues of hair loss and possible prostate morbidity (a contentiously debatable point, to be sure) then come into play. Either way, please make sure to monitor DHT with the transdermals. I’m just not comfortable with gross elevations in DHT, and prefer to avoid adding finasteride whenever possible.
Some have reported an increase in hair growth over the application area(s). All physicians who administer TRT must be prepared to disappoint their patients at this time by pointing out, sadly, this same effect cannot be achieved on the scalp.
TESTOSTERONE PATCHES
These can be quite effective, but are inconvenient to use. Approaching 2/3’s of your patients will develop a contact dermatitis from them at some point. Another drawback is that some patients report they are constantly aware of their placement, and the patches are embarrassingly obvious to other gentlemen in certain public places, such as in the locker room.
The scrotal application variety is the most inconvenient. To see what I would be putting my patients through, I tried them. After just a couple days, I’d had more than enough. Men do not generally enjoy shaving their scrotum, and the patches just do not stay on well anyway. Applying a hair dryer to the patch, as they must be warmed first, is also an annoyance. If you go to the gym during the day, they look strange affixed to the genitals, and must be removed, then reapplied, to shower. They do not stick well in the first place, and even less so once they have been reapplied. Of the two options, I found only the type with the extra adhesive had any chance of remaining in place. The scrotal variety causes the largest increases in DHT—which can be good or bad, as previously explained.
TESTOSTERONE PELLETS
In my opinion, their use is absolutely Stone Age. Sure, they can provide extra revenue by virtue of a billable office based procedure. However, needlessly exposing patients to the risks ALL surgeries pose—hemorrhage and infection—is unwarranted. And the area of insertion will be much tenderer than that following a mere IM injection. But the real issue which selects against pellet implantation is concerned with dosing. Let’s say you establish a “usual” initial dose for the pellets. As will be described in the next section, there is absolutely no way to predict, up front, how a patient will react to a given dose of testosterone, regardless of the delivery system. So you bury these pellets in your patient’s backside, and (hopefully) draw follow-up labs in a month or so. What are you to do if the total testosterone ends up greatly exceeding the top of normal range (meaning the patient hyper-responded to the treatment)? Now you must make a much wider incision to remove them, or a portion of them (and who knows how many to take out?). With their very long half-life, SOMETHING must be done, lest you risk actually damaging the health of the patient by elevating testosterone levels into what might be considered a bodybuilding steroid cycle. And what if the pellets do not elevate T enough? You must bring them back in to implant more, and it’s difficult to sell them on this idea, since they probably are not yet feeling the advantages of TRT enough yet to motivate them into undergoing another surgical procedure. It just doesn’t make sense, to my way of thinking.
Testosterone pellets do have some benefit in that selected patients may believe it more convenient to come in every month or six weeks, and then be done with it for a while. Also, because they release T in a slow, steady rate, the pellets are less likely to induce increases in aromatase activity.
TESTOSTERONE INJECTION
I’ll start out by describing the drawbacks of IM testosterone. They are inconvenient for patients who do not wish to give themselves their own injections, as they must then make weekly trips to your office for same. Why IM test MUST be dosed weekly will be described in detail in another section. Some patients, as you well know, just hate shots (although I have noticed several who had initially claimed this, but admitted, once they had come to enjoy the benefits of TRT, actually came to look forward to their weekly injection). And no doubt, an invasive delivery system brings more risk than, for instance, a testosterone gel or cream (the other best choice for TRT).
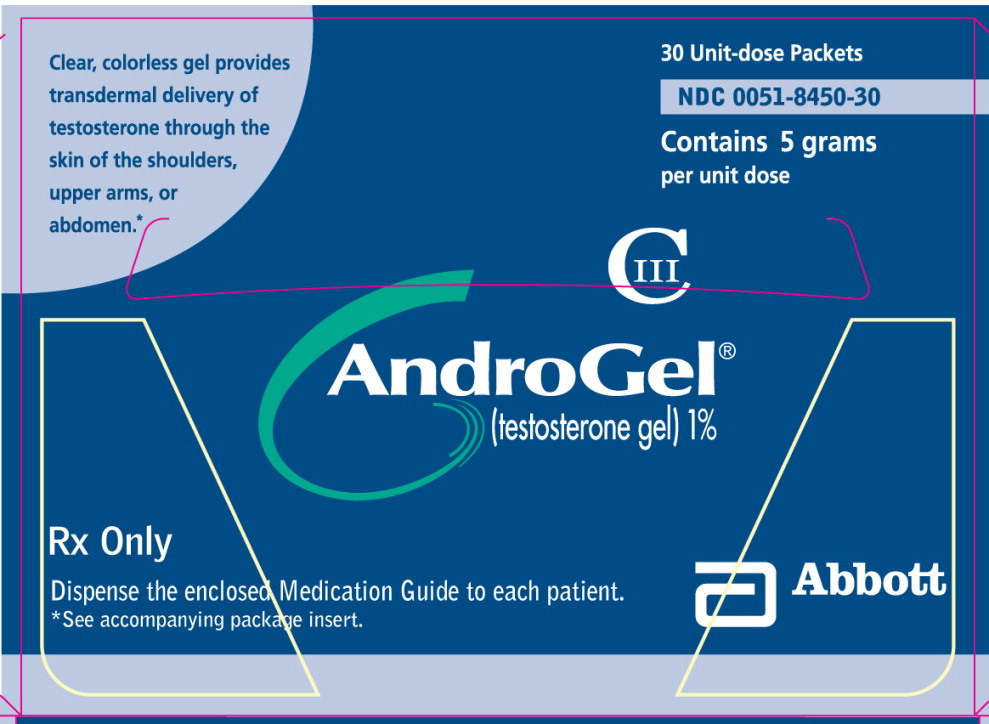
When considering dosing of testosterone cypionate, it is important to remember that, due to the weight of the cypionate ester, a 100mg injection delivers, at best, 70mg of testosterone. This is important to keep in mind when comparing the effects of a 100mg weekly injection of test cyp to the 35mg total dose provided by Androgel 5gms QD over the same period.
HCG
Many practitioners consider this incredible hormone treatment of choice for hypogonadotrophic (secondary) hypogonadism. Such certainly makes sense, as supplementing with a LH analog indeed increases testosterone production in patients who do not concurrently suffer primary hypogonadism. But often, upwards of 1000IU per day must be given to achieve the desired serum T level. Even then, for some unexplained reason, while serum T levels may be adequately elevated, the patients simply do not report realization of the benefits of TRT, when HCG is administered as sole TRT. You also run the risk of inducing LH insensitivity at that dosage, and therefore may actually cause primary hypogonadism while attempting to treat secondary hypogonadism. HCG, especially at higher doses, also dramatically increases aromatase activity, thus inappropriately elevating estrogens. Personally, I recommend never giving more than 500IU of HCG at a time.
A real benefit of HCG is that it will prevent testicular atrophy. I do not think we should ignore the aesthetics of that consideration. Your patients will feel the same way.
OTHER MEDICATIONS
I occasionally hear of physicians trying to use a SERM (Selective Estrogen Receptor Modulator) such as Clomid or Nolvadex, or even an Aromatase Inhibitor (AI), such as Arimidex, as sole “TRT”. All have been shown to elevate LH, and therefore Total Testosterone levels. However, patients report no long-term subjective benefits from these strategies, and the studies thus far reported no long-term changes in lean body mass, fatigue levels, libido, etc. An added risk of using an AI is of driving estrogen levels too low, with deleterious consequences for the lipid profile, calcium deposition, libido, etc.
Finally, Deca-Durabolin (Nandrolone) has no place in TRT. It has a nasty side effect profile, including uncontrollable progesterone-like effects (including gynocomastia) and risk of long-term impotence.
THE MEAT AND POTATOES OF TRT
Now we will delve into the general strategy for administering TRT.
The decision is made, TOGETHER with the patient, which of the various testosterone delivery systems is to be tried first. Be prepared to make adjustments, and try other application methods. You just don’t know which will be best for each particular patient until you try. Besides the simple fact the patient may have a personal preference, or a logistical consideration (i.e. inability/unwillingness to self-inject) for a given application, every-body reacts differently to hormonal manipulation. Some hyper-respond to a given initial dose, others show hardly any bump in serum T levels on same. Yet when you switch to a different delivery system, on initial dosing, they may convert to supraphysiological androgen levels. The same is true of the subjective benefits from TRT. I have patients who love testosterone gel because it successfully treated their ED (the expected outcome because of dramatically increased DHT production), others get more from IM testosterone cypionate. My experience thus far has taught me two lessons: (1) You don’t know how a patient will react to a given dose/system until you try and (2) NOTHING surprises me anymore.
There simply is no way to predict how a particular patient will respond—not Medical History (i.e. number or severity of symptoms), body weight, baseline hormone levels, even anabolic steroid history. I have had very slight gentlemen barely elevate on 100mg of test cyp per week, and massively muscled former steroid athletes who went to nearly two times the top of “normal” range on the same dosage (they had similar baselines). Likewise, one man may see only a modest increase in DHT on 5gms of Androgel, another may become quite supraphysiological on same.
I start my guys out on either testosterone cream/gel 5mgs QD or testosterone cypionate 100mg per week. The IM test cyp must be administered in weekly injections, as opposed to taking twice the dosage every other week. Some physicians even dose every third or fourth week, producing wide swings in serum androgen levels. This puts the patient on an emotional roller coaster, increases the risk of developing polycythemia, greatly accentuates aromatase activity, and actually leaves them lower than they were when they started for the last half of the cycle. In order to get the serum androgen concentration to a stable level more quickly, I “frontload” 200mg the first injection (unless converting over from a gel/cream).
No other medications which manipulate hormone levels are provided until follow-up labs are returned. For IM test cyp patients, the second panel is run following the fifth injection. I also keep in mind the coordination of the injection with the lab draw, as peak serum levels are attained at about the 48 hour point, then fall to about 35% at the one week point. However, by the end of the fifth week, the pharmacodynamics of testosterone cypionate (half life is 5-8 days) are such that relatively stable serum levels are now being produced via weekly injections.
Transdermals can be rechecked in two weeks. They produce stable serum levels, as previously mentioned, for most by the end of the second or third day. Logistically, it makes sense to send the patient for follow-up labs after a fortnight, as there is then time to get the labs back, and bring the patient in, before the initial 30-day supply of the medication runs out. This is better if an adjustment in dosage is mandated by the follow-up labs, or to convert to IM dosing should the patient produce too much DHT. It would be a shame to have the patient refill a script for 5gms of Androgel, when they, by their labs, are going to have their dosage reduced to 2.5gms per day because they hyper-responded to the initial dose, or waste money when what they reallyneed is to be converted to test cyp.
The question of which testosterone delivery system is to be tried first (IM or transdermal) is one which brings much confusion amongst beginning practitioners of TRT.I would, when possible, always start out a patient on a testosterone cream or gel. Ease of application, avoidance of intrusion by injection, and increased probability of successful ED treatment make this so. Also, stable serum levels are attained quickly, determination of successful treatment is more forthcoming (although the manufacturer of this product recommends at least a couple months as adequate trial of therapy). If the labs AND patient’s answers to follow-up subjective report lead to a change to IM testosterone, the conversion is an easy one to make. Simply apply the gel, give the shot, then D/C the gel. However, if a patient is started out on IM test cyp, for instance, yet the patient still does not feel “right” (and thus you may want to try a transdermal delivery system to better raise DHT levels), how are you, given the pharmacodynamics of the testosterone ester, going to safely and successfully dose the conversion to a transdermal?
Dosing changes are made, TOGETHER with the patient, once follow-up labwork is back AND the patient is interviewed regarding their subjective reports of changes in libido, sexual performance, fatigue, strength, mental outlook, etc. Often they will tell you they felt “incredible” the first couple of weeks (and bursting with libido), but they don’t feel quite as good now, but still much better than before they started the TRT. This is because subjective findings are the best while serum androgen levels are accelerating. Adjunctive to this phenomenon is the fact their HPTA was not yet being suppressed, so their endogenous production was higher then than it would be by the end of the month. TRT patients are always HPTA suppressed to greater or lesser degree.
Much weight is placed upon the patient’s subjective findings, as they are not likely to remain compliant in the TRT program unless they feel noticeably better, irrespective of the less obvious long term improvements in CV health, bone density, decreased risk of dementia and cancer, etc. Certainly, if the patient reports they are quite happy at a Total Testosterone level of 600ng/dL, I feel there is little reason to increase their dosage. As an Osteopath, I am loath to provide ANY medication, or increase in dosage, without proven need. As a practical limit, the top of “normal” range for Total Testosterone provides a ceiling, more or less, above which we can expect to find the benefits of TRT beginning to reverse themselves. Actions following androgen receptor binding dramatically improve health and happiness as we go from the hypogonadal state to the top of “normal” range, but beyond that the Lipid Profile and level of insulin sensitivity, for instance, are damaged.
Changes in IM dosing are made in small increments, as response to same is not linear. It is convenient and practical to increase, or decrease IM dosing by 20mg at a time, as this is one “tick mark” on the side of the syringe (for the 200mg/mL concentration). For Androgel patients, we are more limited by their provided dosing whereas we can only either drop down to 2.5gms, or add an extra pack each day (at which time BID dosing may be considered) to reach the 7.5gm, or even 10gm, per day dose. More flexibility is provided through compounded products for those committed to employment of transdermal testosterone delivery systems.
Another risk of jumping the dosage too much is that, should serum androgen levels greatly exceed the top of “normal” range, the patient risks becoming “spoiled” at that level. They would then feel the subjective benefits steroid athletes report, and it would be difficult to get the patient then to be happy at a more moderate—and proper—dose. It is likely you would also therefore produce elevated estrogen activity as well, and further muddy the waters with respect to how the patient feels—and looks (due to emotional changes and even water retention issues from the elevated estrogen). It is far better to make changes in dosing conservatively.
Once the method and dosing is set, by laboratory assay AND subjective report from the patient, then you may address any side effects due to elevated estrogen levels which have occurred. I do not use an AI initially, even when E2 is elevated, because some patients will actually see a drop in estrogen over baseline on follow-up. We would have otherwise added an unnecessary (and relatively expensive) medication. Should the patient develop any “nipple issues” secondary to accelerating serum androgen levels and/or elevated estrogen, you cannot start them on a SERM right away because doing so will invalidate your estradiol assay at follow-up. Of note, males can experience said “nipple issues” even while estrogen levels are within physiological range, due to changes in hormone levels. A drug of the class SERM is treatment of choice in this case, until symptoms subside.
If a patient has “nipple issues”, even while estrogen is within normal range, I add a SERM, emergently. I prefer Nolvadex over Clomid, and Evista is probably best of all for antagonizing estrogen (although much more expensive). Clomid often induces untoward visual effects (i.e. “tracers”), and can cause emotional lability by virtue of its estrogen agonistic effects at the more peripheral (emotion) brain sites. I do like my patients to keep some Nolvadex on hand, should they experience nipple swelling or sensitivity, so they may begin 40mg per day until the symptoms abate, and then taper to 20 mg QD for a few days, then 10mg for a few more, then finally 5mg QD to taper off.
My TRT male patients who suffer E2 elevations above the top of normal range are placed on 0.25mg of Arimidex every third day. If that is not enough, I use the same dose EOD. It is possible to cut the tiny 1mg tabs into quarters, but here a gel or cream preparation, compounded to convenient dosing, makes a lot of sense. A month later I recheck E2, and make further adjustment if necessary. It is important to not lower estrogen too far, which is easy to do with an AI, as doing so has disastrous effects on the Lipid Profile, bone deposition, etc. I prefer to maintain E in mid-range.
So now let’s say we have the patient in a state where Total Testosterone is in the upper quartile of “normal” range, Bioavailable Testosterone is nicely elevated, with E2 safely in check. At this point I offer the patient my HCG protocol. I add in 250-500IU of HCG, on day five, and day six of the week, for those who use the IM injection. In other words, the two days prior to their shot. For those using a transdermal delivery system, every third day. For the IM patients, this compensates for the drop off in serum androgen levels by the half-life of the test cyp. But the main reason is to stave off atrophy of the testicles, by directly stimulating them with the LH analog.
Patients all report they feel dramatically better once the HCG regimen is initiated (and they were properly tuned up on testosterone before they started it). HCG, as a LH analog, increases the activity of the P450 SCC enzyme, which converts CHOL to pregnenolone. Thus all three hormonal pathways are stimulated in patients who may be either entirely, or very nearly, HPTA suppressed. It is my belief this may be a factor in the heightened sense of well-being my patients report throughout the week—far in excess of what a minimal dose of HCG would produce by virtue of induced testosterone production.
Many TRT practitioners add in HCG for a short course every few months, to re-stimulate the testes. My opinion is that it is far better to keep them up to form and function all along the way. The physicians who intermittently use HCG also use it as a “break” in TRT, much the same way hormonally-supplemented athletes manage the typical anabolic steroid cycle. TRT should not be “cycled”. Once I get my patients properly tuned up, I want them to stay that way. They also erroneously believe this allows the HPTA to recover, when it clearly does not. The HCG-induced testosterone production is every bit as suppressive of the HPTA as the TRT, and the supplemented testosterone is still at suppressive serum levels during that time, anyway.
Once the patient is all set, I like to run follow-up labs every six months. It is important to monitor the general health and well-being of the patient, but also insure compliance with treatment protocols and continued effectiveness of same.
My hope is that the preceding diatribe will gainfully assist the practitioner in implementing Testosterone Replacement Therapy regimens for their qualifying patients. Be prepared, however, to blush as they shower you with accolades following their vast improvements in health and happiness. You may even receive thank you notes from their wives!
Please watch for coming articles and books by John Crisler, DO on this, and other, continuing subjects related to anti-aging.
© John Crisler, DO 2004. This article may, in its entirety or in part, be reprinted and republished without permission, provided that credit be given to its author, with copyright notice and www.AllThingsMale.com clearly displayed as source. Written permission from Dr. Crisler is required for all other uses.
About the author
Dr. John Crisler earned a Doctor of Osteopathic Medicine degree from Michigan State University in 2001. Dr. Crisler got his start in hormone modulation and recovery therapies protecting professional and non-professional athletes from the adverse affects of anabolic steroid use. He was the president, founder and CEO of Superior Age Management, AllThingsMale Center for Men's Health in Lansing.

Leave a Reply
You must be logged in to post a comment.