Discussions of the potential role of anabolic-androgenic steroids (AAS) in suicide surfaced recently when AAS and their use among professional athletes were blamed for several suicides of young adult males. These allegations inspired a congressional investigation and renewed anti-steroid rhetoric, but little dispassionate evaluation. The testimony of experts and grieving parents notwithstanding, the role of AAS in suicide is not clear.
Anabolic Steroid Use During Adolescence
The recent tragedies that spurred these investigations involved late adolescent males, yet provoked widespread condemnations of AAS. Problems among adolescent drug users cannot inform issues of adult use (or vice-versa); adolescents are not simply younger adults. Adolescent brains are in transition into the early twenties (Spear, 2000a); these changes initiate and guide the processes normally associated with adolescent/pubertal development (e.g., see Dahl & Spear, 2004). As the brain develops toward its adult configuration, it is awash in endogenous hormones and neuro-chemicals with long-term organizational and functional effects. Drugs that affect this developmental process by impacting these endogenous systems, whether legal, legally prescribed or illicit, can disrupt this process, exerting lasting effects (e.g., Spear, 2000b; Spear, 2002). Testosterone analogs are no exception; androgens have strong organizing effects on the central nervous system (Romeo, 2003). Any drug use, licit or illicit, by adolescents is risky and can have persistent negative effects.
Drug use among Adolescents. Estimates for 2004 suggest that 3.4% of 12th graders have used AAS in their lifetime; 2.5% in the past year and 1.3% in the previous 30 days (Monitoring the Future [MTF], n.d.). In contrast, 76.8% of 12th graders drank alcohol in their lifetime, 70.6% in the past year and 48% in the previous 30 days (MTF, n.d). Rates for most other drugs (e.g., marijuana and cocaine) fall between these estimates and the rates for all drug use tend to increase from 8th to 12th grade. These data suggest that AAS are one of many substances used by adolescents and that their use is relatively rare compared to other drugs, legal and illegal.
Indeed, risky behaviors of all types tend to co-occur and increase across adolescence (Steinberg, 2004) and peak during late adolescence/early adulthood (Middleman, Faulkner, Woods, Emans, & DuRant, 1995). These behaviors are often conceptualized of enhancing adolescents’ individuation from their family of origin, exploration and adoption of adult roles, and gaining access to and acceptance within new social groups (e.g., Jessor, 1991). The increased use of substances is often part of this process (Middleman et al., 1995) and, notably, some researchers suggest that adolescent use of AAS has been “…first and foremost associated with types of problem behavior (i.e., drug [marijuana] involvement and aggressive-type conduct problems) (Wichstrom & Pederson, 2001, p. 10).”
Suicide prevalence. Suicide is a rare event, and, in the absence of a prior attempt, is difficult to predict (a long-discussed issue; e.g., Murphy, 1988; Rosen, 1954). Suicide rates rise with age through adolescence and then fall gain, until the later years; males 75 years and over exhibit the highest rate of suicide (e.g., Pearson & Conwell, 1995), although this pattern may be changing (e.g., Gunnell, Middleton, Whitley, Dorling, & Frankel, 2003). Estimates suggest that from 3 – 11% of adolescents attempt suicide (e.g., Brent, 1995, Lewinsohn, 1994) and suicide is the third leading cause of death in adolescents aged 15 – 24 years (Goldsmith, Pellmar, Kleinman, & Bunney, 2002). In 1990, about 13.2 completed suicides occurred per 100,000 adolescents in the 15-24 age range (Woods, Lin, Middleman, Beckford, Chase, & Durant, 1997). Suicide rates among 15-19 year olds and 15-24 year olds have increased over the last several decades (Guyer, MacDorman, Martin, Peters, & Strobino, 1998; Woods et al., 1997) and the rate of attempts increases into the late teen and early twenties (Gould & Kramer, 2001; Wichstrom, 2000).
Suicide Risk Indicators. A wide range of characteristics is associated with increased suicide probability (e.g., Ayyash-Abdo, 2002; Woods et al., 1997). For example, a history of previous attempts (Wichstrom, 2000), physical fights in the past 12 months and gun carrying, (Woods et al., 1997), depression (Ayyash-Abdo, 2002; Boergers, Spirito, & Donaldson, 1998), and hopelessness (e.g., Ayyash-Abdo, 2002) are associated with adolescent suicide attempts. In addition, substance use (e.g., Ayyash-Abdo, 2002, Woods et al., 1997), low self-esteem (e.g., Wichstrom, 2000), peer/family member suicide/attempt (e.g., Brent, 1995), socially prescribed perfectionism (e.g., Boergers et al., 1998), and alcohol intoxication (e.g., Wichstrom, 2000) are also associated with adolescent suicide. Approximately 28% of suicides by children 8-15 years have been attributed to alcohol (Center for Substance Abuse Prevention [CSAP], 2002). Brower has commented that suicide is the third leading cause of death among 15-24 year olds and suggested that “This…age group…is already at high risk…when you add steroids you are increasing the risk of suicide (University of Michigan Health Systems, 2005).” As noted above, a vast array of individual characteristics, related to both negative affect and risk taking, are associated with increased suicide risk in this age group, including the use of many substances (e.g., alcohol, CSAP, 2002; prescription antidepressants; Garland, 2004).
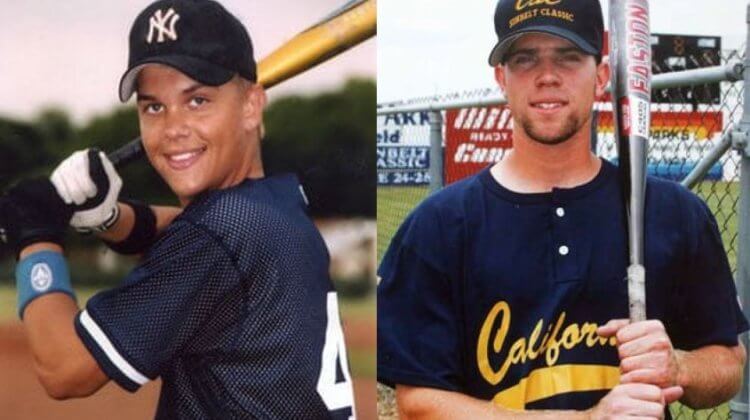
The Recent Cases. An in-depth exploration of the recent tragedies is not the point of this review nor is this brief review meant to denigrate these young men or deny their families’ grief. However, a brief review of the published material covering the two most publicized cases might be informative about the issue involved. Such a review tends to replicate the findings noted above. Taylor Hooton reportedly “colored his hair and looked twice when he passed a mirror (Longman, 2003)” and “…was always concerned about his looks (Kix, 2004). In combination with a reported desire to be bigger suggests potential body dissatisfaction (e.g., Pope, Phillips, & Olivardia, 2000) which is associated with both AAS use (Cafri, Thompson, Ricciardelli, McCabe, Smolak, & Yesalis, 2005) and suicide (as a form of “socially-prescribed perfectionism”; Boergers et al., 1998). He had “low self-esteem” (Longman, 2003), a family history of depression (mother) and suicide attempt (sister) (Longman, 2004) and was taking anti-depressant mediation (Lexapro) (Ardis, 2005). [Interestingly, a Mail Tribune (8-10-2004) headline (Landers, 2004) seemed to echo the parents’ sentiments in these cases, reading “Drug leads to son’s suicide, family says” – but it was actually referring to Lexapro. See both Garland, 2004 and Valuck, Libby, Sills, Giese, & Allen, 2004 for a discussion of antidepressants and adolescent suicide]. His AAS use was allegedly motivated by wanting to excel at baseball (Numerous sources including father’s testimony), although some sources have suggested it had more to do with personal appearance and status.
If such a case history could truly prove causation, then the brief review above has identified several potential “causes”. But such a “psychological autopsy”, which is commonly used to investigate suicides, cannot show causation. It can suggest that many warning signs can be identified, any one (or combination) of which might be associated with suicide, but none of which can be definitively shown as a cause. In this case, to single out one might reflect other than scientific issues.
Another of the young men, Rob Garibaldi, was on medication for attention deficit hyperactivity disorder (ADHD; Klein, 2005) and depression (Fainaru-Wada, 2004; Klein, 2005), and, according to friends, engaged in periods of marijuana and alcohol use concurrent with AAS use (Fainaru-Wada, 2004). His manner of death (gunshot) also suggests risk (Woods et al., 1997). His AAS use was also motivated by the desire for a career in baseball (parental testimony), again suggesting body dissatisfaction issues, perhaps externally reinforced (Fainaru-Wada, 2004). All of these factors, including AAS use, suggest increased risk – to assert that any one of them was a single cause reflects a confirmation bias.
Many individual difference factors, including long-term and current use of a range of substances, characterize the history of suicide completers. Although an in-depth review of these cases is beyond the scope of this paper, a brief reading suggests that numerous factors known to be associated with teen suicide were present in these cases – several others were likely present as well. In fact, relevant to both of these cases, AAS researcher Harrison Pope is noted as suggesting that “…a steroid user who was also taking antidepressants for an existing depressive illness might be more susceptible to suicide risk (Klein, 2005)”. The characteristics present in these cases might be causes, effects of other causes, or correlates – such a research design cannot different these possibilities. For example, the factors that might motivate AAS use (e.g., low self-esteem, body dissatisfaction) might also “predict” suicide, and at best, the temporal relationship to AAS use might suggest that they exert a “permissive effect (Sapolsky, 1997, p. 153)” rather than a causal one, which, in the example of testosterone-related aggression, suggests that “”…testosterone is not causing aggression, it’s exaggerating the aggression that’s already there (italics in the original; Sapolsky, 1997, p. 155).” A similar effect is plausible in the case of suicidal behavior as well and research suggests that a wide range of substances might exert similar effects (e.g., antidepressants; Garland, 2004; alcohol; CSAP, 2002).
In addition, the link between AAS use/withdrawal and suicide in both the larger literature (e.g., Brower, Blow, Eliopolis, & Beresford, 1989) and in these cases is predicated on idea that depression is associated with AAS withdrawal and that suicide is a consequence of that depression (whether such post AAS use depression is solely caused by AAS withdrawal is hardly a proven fact). This association is noted as proof that these suicides were caused by AAS use. However, researchers have also suggested that, in adolescents, suicide might also be considered as part of the constellation of risky and problem behaviors that appear in adolescence (e.g., Woods et al., 1997), which also includes drug use. This may represent a case of unwarranted application of results from adults to explain suicidal behavior in adolescents.
Can or should these cases inform policy on adult use of AAS? As noted above, research from adolescents cannot indiscriminately be applied to adults, or vice-versa. Hence, although these cases serve to indict AAS use by teenagers, it is already well established that use of any drug by adolescents is a risky proposition and is associated with an increased risk of suicide. This has little to do with the question of AAS use or withdrawal as a cause of suicide among adult AAS users.
Anabolic Steroids and Suicide in Adults.
Although frequently mentioned in popular periodicals during the past several months, the peer-reviewed literature associating between AAS withdrawal with suicide is fairly limited. A literature search of the Psycinfo data base (6-30-05), using the terms “suicide” and “Anabolic-androgenic steroids” in the title or abstract of studies with humans published in peer-reviewed journals yielded 4 papers, including one oft-cited letter to the editor (Brower, et al., 1989).
Brower noted “The most frequently described adverse psychiatric effects of AAS are extreme mood swings ranging from mania to depression, suicidal thoughts and behaviors, marked aggression… Mania…violent aggression and delusions are most likely to occur during a course of AAS use, whereas depressive episodes and suicide attempts are most likely to occur…during AAS withdrawal” (italics added; testimony of Kirk Brower to Congress, 3/17/2005). This accurately notes that these are rare effects and, in those rare instances when they appear, they do so at specific times in the AAS use/withdrawal process. Of course, when congressmen, distraught family members, and a society at war with drugs see the terms “frequently” and “most likely” they frequently are likely to read them as suggesting that mania, aggression, depression and suicide are probable during AAS use/withdrawal. Recent experimental research found that 3.2% (1 of 31) of men in whom subnormal androgen levels were induced (an experimental analog for acute AAS withdrawal) exhibited major depression (Schmidt et al., 2004). The authors note that “Few subjects…developed negative mood symptoms during an otherwise dramatic albeit brief…withdrawal and replacement of testosterone. (p. 1001)”, “Baseline level of symptomatology appeared to differentiate the men’s responses to hormone withdrawal and replacement (p. 1002)” and “Our data fail to support a uniform adverse effect on mood of induced hypogonadism in healthy young men (p. 1003)”. This study deserves further examination, but space precludes that effort here. Suffice to say, in randomly assigned (note this means that these men did not choose for their own personal reasons to use a drug) healthy young men (aged 23 – 46 years), an experimental analog to AAS withdrawal caused negative mood symptoms in few participants, and baseline individual differences appeared to influence the response of those affected. Experimental studies with AAS consistently tend to report similar findings – individuals administered AAS, as opposed to those who freely choose to abuse them – tend to exhibit fewer psychological effects (see Darkes, n.d.).
In the case of suicide, 3.9% of a sample of 77 those classified as AAS users reported attempting suicide during withdrawal (Malone, Dimeff, Lombardo, & Sample, 1995) and 1 of 24 AAS users interviewed in a substance use treatment facility (not a representative sample of AAS users but abusers and abusers of other substances as well) had attempted suicide during withdrawal (Kanayama, Cohane, Weiss, & Pope, 2003). Nonetheless, some researchers have characterized suicide attempts during AAS withdrawal as “…more common than most people suspect” (Pope quoted by Longman, 2003). Lifetime prevalence estimates for AAS use in males are somewhere in the one million range (e.g., Cowart & Yesalis, 1998) and the rates reported in the above studies (in one case; Kanayama et al., 2003, with abusers in treatment, not typical users), this outcome hardly seems common at all. It is certainly devastating when it happens, but it is not common – in fact, these reports suggest it is statistically rare. Of course, even if the percentage of AAS users attempting suicide during withdrawal were higher, case study methodology cannot show a causal relationship and note that these researchers do fall short of attributing the deaths to AAS. AAS use may be one of many risk factors, but it is unclear which of those many characteristics might play a part in individuals’ choices to use AAS or their suicidal behavior.
For example, one hypothesis suggests that AAS use is motivated by muscle dysmorphia (Cafri et al., 2005; Pope et al., 2000). Such body image disturbances are also associated with poor self-esteem and other factors associated with suicide. Hence, some users might bring with them arrange of possible predispositions to psychopathology and suicide prior to any AAS use. And, if users do not manage withdrawal effectively (which is difficult given the status of these drugs), they may lose prized muscle, also leading to depression, hopelessness and increased risk for suicide in those with such concerns. Hence, AAS withdrawal may involve depression and potential suicide which are secondary to AAS use, related to many other factors that are involved in the decision to use AAS and the subsequent effects – such that the causes are not so clear.
The existing research on suicide in AAS users relies on case studies (e.g., Brower et al., 1989; Kanayama et al., 2003; Thiblin et al., 1999) that examine the characteristics of completed suicides, much as was done briefly above in the recent cases. However it has been noted that “Case studies are commonly used to describe the association of abuse of AAS with the most unexpected, severe and dramatic disease conditions. Such reports must be interpreted with caution. They are characterized by describing a possible relationship between AAS administration and the disease condition and, since evidence is lacking, may exaggerate the problem (Hartgens & Kuiper, 2004, p. 517).” That is, although they are the best available method for looking at the characteristics associated with rare events and can suggest associations among events occurring together, such as suicide, depression, alcohol use, etc.; they are likely to suggest that a problem is worse than it is. The testimony to congress and many reports (e.g., Brower et al., 1989a; 1989b; Malone & Dimeff, 1992) on AAS withdrawal and suicide reflect such information; they alert us to important signs and suggest when precautions should be taken, but they seemingly overstate the problem and are not proof that a causal relationship exists. In fact, few published studies on the effects of AAS in general meet scientific standards for such an inference (Hartgens & Kuiper, 2004).
A look at one such study (Thiblin et al., 1999) illustrates the approach. Eight suicides (from 1988-1997) were identified as AAS users based on anthropomorphic examination (e.g., muscle mass, testicular atrophy) and partners/parents of the deceased provided historical information (we will not discuss the potential biases involved in such an approach, but they obviously exist). Most cases exhibited at least one of the established correlates of suicide risk (e.g., history of other substance abuse, psychological problems, or suicide by family member/close peer). One case had ceased AAS use 6 months (3 months is considered the typical window; e.g., Brower et al., 1989; Pope & Katz, 1988) prior to committing suicide and his ex-girlfriend had recently started dating another man. Although no obvious mention of the total number of suicides over that time period was made, in one geographical sub-area 150 male suicide victims aged 21-35 years were examined and three AAS user cases (2%) were identified.
Although the cases reviewed showed many signs of suicide risk and there was no non-suicidal AAS user controls, the authors concluded that “Long-term use of AAS seems to increase the risk of suicide in several ways” and that “…current mental and behavioral changes with a conceivable relation to the use of AAS led to psychosocial complications that in turn precipitated the suicides (p. 230).” This is clearly a prime example of the “exaggeration of the problem (Hartgens & Kuiper, 2004, p. 517)” that results from such studies.
Studies of attempted or completed suicides cannot determine what “caused” that suicide (other than the proximal cause of death in completed suicides); “Whether these individuals were predisposed to suicide before their steroid use or whether they developed suicidal depressions because of their steroid use is unclear (Brower, et al., 1989, p. 1075).” Nonetheless, the idea that AAS (or withdrawal) causes suicide persists and is accepted publicly as proven. The above shows that suicide is affected by many different influences, including personal factors, the familial/social environment, and media exposure (e.g., the ecological model; Ayyash-Abdo, 2002). Prospectively identifying those who will later commit suicide leads to a large number of false-positives (e.g., Murphy, 1988). Suicidal individuals share many characteristics with their non-suicidal peers; we can learn the characteristics of those who commit suicide by examining their histories, but cannot know what factors are the most likely causes of suicide without knowing the prevalence of those factors in non-suicidal people. Case studies and psychological autopsies, at best, can describe the characteristics of someone who succeeded in committing suicide and alert us to indicators of risk. And the above can be asserted to do that; AAS withdrawal may or may not cause suicide, but the possibility of suicide during withdrawal cannot be neglected – precautions are warranted.
Should the Risk of Suicide be used to Indict Steroid use in Healthy Adults?
The larger literature on the psychological effects of AAS is large and spans many years; the portion of it focusing on withdrawal and suicide is more limited. Much of that larger literature does not meet scientific standards (e.g., Darkes, n.d.; Hartgens & Kuiper, 2004). These scientific shortcomings have not tempered the sweeping statements regarding AAS as causal agents of inevitable negative outcomes made by the press and some scientists. These shortcomings do not make what is known about AAS use irrelevant by any means; parents, teachers, coaches and others have children to rear, teach or mentor and they need all the help that research can provide. Those who choose to use AAS need to be aware of the possible consequences and exercise vigilance. We cannot, however, take this research as valid evidence that deleterious effects and outcomes, including AAS use, and occur in concert with it, are inevitably caused by AAS use.
We also cannot generalize what we know about adults to adolescents and vice-versa. Adolescents are not merely younger adults – adolescence is a time of great transition. This is not a revelation – our society has long enacted laws prohibiting adolescents/young adults from using certain substances (e.g., tobacco, alcohol) and engaging in certain behaviors (e.g., driving, marrying, voting, volunteering for military service) that are legal for adults, in recognition of adolescent development. Of course, age is only a number and a given number does not mean the transition has ended – the changes do not track linearly with age. For various reasons, some adults are no better suited for certain behaviors or the use of certain substances than are adolescents (e.g., adult DUIs are quite prevalent and some AAS abusers do commit hostile or suicidal acts). But such laws reflect our society’s belief that, at a certain point in development, individuals become competent to make choices and handle consequences. For instance, the best known, yet legal, of these “forbidden” substances, alcohol, has shown strong associations with both aggression (e.g., Hoaken & Stewart, 2003) and suicide (Wichstrom, 2000), yet is legal for adults to use with penalties in place for illegal behavior. In addition, with alcohol, we clearly draw a line between use and abuse. It is unclear whether this is a matter of tradition, constituency, or power, but such conundrums deserve further consideration.
Consider also that several studies suggest that AAS use is associated with the use of multiple drugs among adolescents (e.g., DuRant, Escobedo, & Heath, 1995; DuRant, Rickert, Ashworth, Newman, & Slavens, 1993), while Malone et al. (1995) suggest that “Concurrent use of psychoactive drugs other than AAS does not appear to be common in intensively training weight lifters and bodybuilders (p. 25)”. This suggests what should already have been surmised; AAS use is a different phenomenon in adults and adolescents and the ultimate motivation for using AAS in these groups differs greatly. This is especially relevant in light of the recent explorations of therapeutic uses of androgens (e.g., androgen replacement therapy; Bhasin & Bremner, 1997; male contraception; O’Connor, Archer, & Wu, 2004l AIDS wasting; Volkow, 2005).
Suicide is a devastating and tragic event and the more that is known about the individual characteristics that signal increased risk for suicide, especially in adolescents, the better equipped we will be to intervene in time to save innocent lives like those mentioned herein. Suicide is an event where false-positive identification carries with it little harm at the personal level (certainly much less than the act, especially if handled correctly to avoid any stigma), but great benefit in some cases. Efforts to educate adolescents, families, physicians and others to the warning signs, be they drug use or other risky behaviors or psychopathologies, should be applauded. Efforts to ascribe such events to a single cause can distract attention from other important indicators that need to be noted. Ascribing blame can be comforting at times of devastation when one desperately needs to make sense of events and “do something”. But, from a scientific perspective, such efforts must be looked at skeptically and dispassionately. In this scientists must strive to remain ethically neutral and objective. They must attempt to ensure that they communicate clearly, not adjusting their message for a public seeking confirming statements and value judgments. Science has limitations, as do its research methods. Scientists do their best service when they remember this when reporting on their work to the public.
References
Ardis, C. (2005). Steroids can lead to many problems. The Monitor – www.themonitor.com, 3-29-2005. Accessed on 7/14/2005 at http://www.themonitor.com/SiteProcessor.cfm?Template=/GlobalTemplates/Details.cfm&StoryID=6424&Section=Chris%20Ardis.
Ayyash-Abdo, H. (2002). Adolescent suicide: An ecological approach. Psychology in the Schools, 39, 459-475.
Bhasin, S., & Bremner, W.J. (1997). Emerging issues in androgen replacement therapy. Journal of Clinical Endocrinology and Metabolism, 82, 3-8.
Boergers, J., Spirito, A., & Donaldson, D. (1998). Reasons for adolescent suicide attempts: Associations with psychological functioning. Journal of the American Academy of Child & Adolescent Psychiatry, 37, 1287-1293.
Brent, D.A. (1995). Risk factors for adolescent suicide and suicidal behavior: Mental and substance use disorders, family environmental factors and life stress. Suicide and Life-Threatening Behaviors, 25(suppl), 52-63.
Brower. K.J. (2005). Testimony to congress on 3/17/2005. Accessed on 7/14/2005 and accessible at http://reform.house.gov/UploadedFiles/Brower%20Testimony.pdf.
Brower, K.J., Blow, F.C., Eliopolis, G.A., & Beresford, T.P. (1988). Anabolic androgenic steroids and suicide. American Journal of Psychiatry, 146, 1075.
Cafri, G., Thompson, J.K., Ricciardelli, L., McCabe, M., Smolak, L., & Yesalis, C. (2005). Pursuit of the muscular ideal: Physical and psychological consequences and putative risk factors. Clinical Psychology Review, 25, 215-239.
Center for Substance Abuse Prevention. (2002). Suicide, depression, and youth drinking. Prevention Alert, 5 (17). Accessed on 7/14/2005 and accessible at http://media.shs.net/prevline/pdfs/suicide2002.pdf.
Dahl, R. E. & Spear, L. P. (Eds.) (2004). Adolescent Brain Development: Vulnerabilities and Opportunities (Annals of the New York Academy of Sciences, Vol. 1021); New York: New York Academy of Sciences, 2004.
Darkes, J. (n.d.). Anabolic/Androgenic Steroid Use and Aggression I: A Review of the Evidence. Accessed 7/14/2005 and accessible at http://mesomorphosis.com/articles/darkes/anabolic-steroids-and-aggression-01.htm.
DuRant, R.H., Escobedo, L.G., & Heath, G.W. (1995). Anabolic-steroid use, strength training, and multiple drug use among adolescents in the United States. Pediatrics, 96, 23-28.
Durant, R.H., Rickert, V.I., Ashworth, C.S., Newman, C., & Slavens, G. (1993). Use of multiple drugs among adolescents who use anabolic steroids. New England Journal of Medicine, 328, 922-926.
Fainaru-Wada, M. (2004). Dreams, steroids, death – a ballplayer’s downfall. San Francisco Chronicle [SFC] December 19, 2004. Accessed on 7/14/2005 and accessible at http://www.sfgate.com/cgi-bin/article.cgi?f=/c/a/2004/12/19/MNG14AEB7S1.DTL&hw=garibaldi&sn=001&sc=1000.
Garland, E.J. (2004). Facing the evidence: Antidepressant treatment in children and adolescents. Canadian Medical Association Journal, 170, 489-491.
Goldsmith, S. Pellmer, T., Kleinman, A., & Bunney, W. (2002). Reducing suicide: A national imperative. Washington DC: The National Academies Press.
Gould, M.S., & Kramer, R.A. (2001). Youth suicide prevention. Suicide and Life-Threatening Behavior, 31(suppl), 6-31.
Gunnell, D., Middleton, N., Whitley, E., Dorling, D., & Frankel, S. (2003). Why are suicide rates rising in young men but falling in the elderly? – A times series analysis of trends in England and Wales 1950-1998. Social Science in Medicine, 57, 595-611.
Guyer, B., MacDorman, M.F., Martin, J.A., Peters, K.D., & Strobino, D.M. (1998). Annual summary of vital statistics – 1997. Pediatrics, 102, 1333-1349.
Hartgens, F., & Kuipers, H. (2004). Effects of androgenic-anabolic steroids in athletes. Sports Medicine, 34, 513-554.
Hoaken, P.N.S., & Stewart, S.H. (2003). Drugs of abuse and the elicitation of human aggressive behavior. Addictive Behaviors, 28, 1533-1554.
Jessor, R. (1991). Risk behavior in adolescence: A psychosocial framework for understanding and action. Journal of Adolescent Health, 12, 597-605.
Kanayama, G., Cohane, G.H., Weiss, R.D., & Pope, H.G. (2003). Past anabolic-androgenic steroid use among men admitted for substance abuse treatment: An underrecognized problem? Journal of clinical Psychiatry, 64, 156-160.
Kix, P. (2004). All the rage. Dallas Observer [DO], 08-12-2004. Accessed on 7/14/2005 and accessible at http://web.lexis-nexis.com/universe/document?_m=f29c6f0b6ebb234df0c3c59b41f27e08&_docnum=90&wchp=dGLbVtz-zSkVA&_md5=a2447f447d9ba749226808b70434d926.
Klein, G. (2005). Athlete’s parents see steroid link in death. Los Angeles Times [LAT], 03-16-2005. Accessed on 7/14/2005 and accessible at http://proquest.umi.com/pqdweb?index=143&did=…&aid=1.
Landers, M. (2004). Drug leads to son’s suicide, family says. The Mail Tribune (8-10-2004). Accessed on 7/14/2005 and accessible at http://www.mailtribune.com/archive/2004/0810/local/stories/07local.htm.
Lewinsohn, P.M., Rohde, P., & Seeley, J.R. (1994). Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology, 62, 297-305.
Longman, J. (2003) Drugs in sports: An athlete’s dangerous experiment. New York Times 11-26-2003. Accessed on 7/14/05 and accessible at http://web.lexis-nexis.com/universe/document?_m=61cfff3804b3b5f27fdd52e87eca6a4b&_docnum=117&wchp=dGLbVtz-zSkVA&_md5=63863702b68b33f02241348f0bedb3d8.
Malone D.A., & Dimeff, R.J. (1992). The use of fluoxetine in depression associated with anabolic steroid withdrawal: A case series. Journal of Clinical Psychiatry, 53, 130-132.
Malone, D.A., Dimeff, R.J., Lombardo, J.A., & Sample, R.H. (1995). Psychiatric effects and psychoactive substance use in anabolic-androgenic steroid users. Clinical Journal of Sports Medicine, 5, 25-31.
Middleman A.B., Faulkner A.H., Woods E.R., Emans S.J., & DuRant R.H. (1995). High-riskbehaviors among high school students in Massachusetts who useanabolic steroids. Pediatrics, 96, 268-272.
Monitoring the Future 2004 data. (n.d.) Retrieved July 13th, 2005 and accessible at http://www.monitoringthefuture.org/data/data.html.
Murphy, G.E. (1988). The prediction of suicide. In Lesse, S (Ed.) What We Know about Suicidal Behavior and How to Treat it. Northvale, NJ, US: Jason Aronson, Inc.
O’Connor, D.B., Archer, J., & Wu, F.C.W. (2004). Effects of testosterone on mood, aggression, and sexual behavior in young men: A double-blind, placebo-controlled, cross-over study. Journal of Clinical Endocrinology and Metabolism, 89, 2837-2845.
Pearson, J.L., & Conwell, Y. (1995). Suicide in late life: Challenges and opportunities for research. International Psychogeriatrics, 7, 131-136.
Pope, H.G., & Katz, D.L. (1988). Affective and psychotic symptoms associated with anabolic steroid use. American Journal of Psychiatry, 145, 487-490.
Pope, H.G., Phillips, K.A. & Olivardia, R. (2000). The Adonis Complex: The Secret Crisis of Male Body Obsession. New York, NY; Free Press.
Romeo, R.D. (2003). Puberty: A period of both organizational and activational effects of steroid hormones on neurobehavioural development. Journal of Neuroendocrinology, 15, 1185-1192.
Rosen, A. (1954). Detection of suicidal patients: An example of some limitations in the prediction of infrequent events. Journal of Consulting Psychology, 18, 397-403.
Sapolsky, R.M. (1997). The Trouble with Testosterone and Other Essays on the Human Predicament. Scribner: New York, NY.
Schmidt, P.J., Berlin, K.L., Danaceau, M.A., Neeren, A., Haq, N.A., Roca, C.A., & Rubinow, D.R. (2004). The effects of pharmacologically induced hypogonadism on mood in healthy men. Archives of General Psychiatry, 61, 997-1004.
Spear, L. P. (2000a). Neurobehavioral changes in adolescence. Current Directions in Psychological Science, 9, 111-114.
Spear, L.P. (2000b). The adolescent brain and age-related behavioral manifestations. Neuroscience and Behavioral Reviews, 24, 417-463.
Spear, L.P. (2002). The adolescent brain and the college drinker: Biological basis of propensity to use and misuse alcohol. Journal of Studies on Alcohol, suppl. 14, 71-81.
Steinberg, L. (2004). Risk taking in adolescence: What changes and why?. In R.E. Dahl, & L.P Spear (Eds.) Adolescent Brain Development: Vulnerabilities and Opportunities. Annals of the New York Academy of Sciences, Vol. 1021); New York: New York Academy of Science.
Thiblin, I., Runeson, B., & Rajs, J. (1999). Anabolic androgenic steroids and suicide. Annals of Clinical Psychiatry, 11, 223-241.
University of Michigan Health System. (2005). ‘Roid rage, depression and suicide: U-M addiction expert warns of dangers of teen steroid use. UMHS Health E-News, April, 2005. Accessed on 7/14/2005 and accessible at http://www.med.umich.edu/health-e_news/apr2005/hottopics.html.
Valuck, R.J., Libby, A.M., Sills, M.R., Giese, A.A., & Allen, R.R. (2004). Antidepressant treatment and risk for suicide attempt buy adolescents with major depressive disorder: A propensity-adjusted retrospective cohort study. CNS Drugs, 18, 1119-1132.
Volkow, N.D. (2005). Testimony to congress on 3/17/2005. Accessed on 7/14/2005 and accessible at http://reform.house.gov/UploadedFiles/Volkow%20Testimony.pdf.
Wichstrom, L. (2000). Predictors of Adolescent Suicide Attempts: A Nationally Representative Longitudinal Study of Norwegian Adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 39, 603-610.
Wichstrom L., and Pederson, w. (2001). Use of anabolic-androgenic steroids in adolescence: Winning, looking good or being bad? Journal of Studies on Alcohol, 62, 5 – 13.
Woods, E.R., Lin, Y.G., Middleman, A., Beckford, P., Chase, L., & DuRant, R.H. (1997). The Associations of Suicide Attempts in Adolescents. Pediatrics, 99, 791-796.
Yesalis, C., & Cowart, V. (1998). The Steroids game.. US: Human Kinetics.
About the author
Jack Darkes, Ph.D. is a Clinical Psychologist and currently the Director of the Psychological Services Center in the Department of Psychology at the University of South Florida. He is well-known and respected both nationally and internationally for his research on psychological factors related to substance use and abuse. He has applied his experience to an examination of the use and behavioral effects of anabolic-androgenic steroids (AAS) and his writings on AAS are well-known to readers of various internet fitness and bodybuilding websites.
Leave a Reply
You must be logged in to post a comment.