Once-weekly PEGylated recombinant human growth hormone (rhGH) is the sole long-acting GH formulation available currently for pediatric patients with GH deficiency (GHD). The aim of this study was to evaluate the efficacy and safety of PEGylated rhGH ...

www.ncbi.nlm.nih.gov
A couple distinctions between this study's population vs. ours & between IGF-I vs. SDS should be made.
First, going from sub-normal IGF-I standard deviation score (-1.24 SDS) to normal (1.09 - 1.26 SDS) in the case of Growth Hormone Deficiency children (childhood GHD) is qualitatively different than going from normal to acromegalic IGF-I (as SDS, or raw) in the case of rhGH-using bodybuilders are not actually closely comparable.
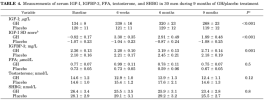
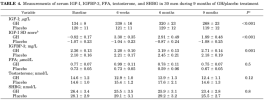
Any decrement that does (in fact) occur at 4 - 5 mo, but with sampling at 6, 12, and 24 mo, will still result in an improved health outcome in GHD children & ΔIGF-I (raw), despite there in fact being this significant decrement in GH response (Δ IGF-I)... by 6 months, to the tune of -11%, and by 9 months to the tune of
-42% in a more valid comparison population to bodybuilders, of healthy but abdominally obese men given 2.85 IU * 100 kg⁻¹ body weight daily.
[1].
SDS (Standard Deviation Scores) require explanation because these cannot be viewed the same as a raw IGF-I value for the purpose of comparison. SDS are intended to describe dispersion about the mean for a population's IGF-I in terms of the Z-score. Since distribution of IGF-I values in a healthy population is non-Gaussian, mathematical transformation is necessary to obtain reference intervals for each age group. Here, that population must include healthy Chinese children; whose IGF-I levels differ significantly from other populations, e.g., even between Caucasian population-wide data there is considerable variation in IGF-I concentrations.
This ties in to the impact of known heritable factors (i.e., genes and genotypes) on GH response (Δ IGF-I). Take the GHR gene that controls the expression of GH receptor in our bodies. Its d3 homozygous genotype (those that are d3d3) see substantially increased IGF-I, far greater than in those d3fl and especially flfl. These differences likely underlie why some individuals see rapid increases in IGF-I at initiation versus others seeing little change (hypo- or even non- responders). Besides GHR genotype, rhGH dose & age at diagnosis (e.g., Growth Hormone Deficiency) affect the Δ IGF-I at 6, 12, & 24 mo.
In some populations, the d3 homozygous (d3-GHR) genotype has a prevalence of > 50%!
Important general considerations that arise out of the use of SDS to describe IGF-I distribution are that:
1. Data is not applicable to BMI > 28 kg/m² (i.e., bodybuilders), or those on exogenous estrogens (especially oral estrogens); e.g., excluding exogenous estrogen use yielded IGF-I in women > than in men, until age 50 (menopause).
2. Use of different populations is the greatest source of variation.
3. Lack of specificity (i.e., IGFBP interference removal; specificity and/or affinity to the IGF-I antibody used) arises as a source of variation, with significant implications for patients with disorders that affect IGFBP profile, such as acromegaly (analogous to high dose rhGH use) or chronic kidney disease.
The very fact of this study's failing to describe a significant decrement in its proxy for IGF-I (raw) – (I have not sought out its supplementary materials for more for more particularized data on SDS vs. months followup) – vis-a-vis rhGH use belies its insufficient sensitivity & power for this task.
References
[1] Johannsson G, Mårin P, Lönn L, Ottosson M, Stenlöf K, Björntorp P, Sjöström L, Bengtsson BA. Growth hormone treatment of abdominally obese men reduces abdominal fat mass, improves glucose and lipoprotein metabolism, and reduces diastolic blood pressure. J Clin Endocrinol Metab. 1997 Mar;82(3):727-34. doi: 10.1210/jcem.82.3.3809.