malfeasance
Member
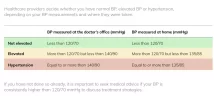
"For the second, published Oct. 29, 2016, in The Lancet, researchers analyzed data from CLARIFY, a registry of more than 22,600 people with heart disease from 45 countries. They determined that, compared with people who had systolic blood pressure of 120 to 139 mm Hg and diastolic pressure of 70 to 79, people with a systolic blood pressure of 140 mm Hg or higher were more likely to experience heart attacks or strokes, to be hospitalized with heart failure, or to die within a five-year period. But the same was true for heart attacks, heart failure, and death in people with low blood pressure (systolic pressure below 120 mm Hg and diastolic pressure under 70 mm Hg).
In an analysis published online April 5, 2017, by The Lancet, German researchers pooled data from two clinical trials involving 31,000 men and women ages 55 or older who had cardiovascular disease or advanced diabetes. Participants were assigned to take either ramipril (Altace), telmisartan (Micardis, Activin), both drugs, or neither drug for about five years. The researchers determined that systolic pressures below 120 mm Hg and diastolic pressures below 70 mm Hg were associated with an increased risk of dying from heart disease or any cause compared with systolic pressures between 120 mm Hg and 140 mm Hg and diastolic pressures between 70 and 80 mm Hg. Diastolic pressures of less than 70 mm Hg were also associated with an increased risk of having a heart attack and hospitalization for heart failure."

 www.health.harvard.edu
www.health.harvard.edu
In an analysis published online April 5, 2017, by The Lancet, German researchers pooled data from two clinical trials involving 31,000 men and women ages 55 or older who had cardiovascular disease or advanced diabetes. Participants were assigned to take either ramipril (Altace), telmisartan (Micardis, Activin), both drugs, or neither drug for about five years. The researchers determined that systolic pressures below 120 mm Hg and diastolic pressures below 70 mm Hg were associated with an increased risk of dying from heart disease or any cause compared with systolic pressures between 120 mm Hg and 140 mm Hg and diastolic pressures between 70 and 80 mm Hg. Diastolic pressures of less than 70 mm Hg were also associated with an increased risk of having a heart attack and hospitalization for heart failure."

Can your blood pressure be too low? - Harvard Health
In people with heart disease, lowering diastolic blood pressure (the bottom number) to less than 70 mm Hg may increase the risk of heart attack, heart failure, and death....