Anonymous35
Member
Yes but rosuvastatin with bad kidney like mine can accumulate and then as a result rhabdo
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
Yes but rosuvastatin with bad kidney like mine can accumulate and then as a result rhabdo
Never knew. ThanksDefine "Good" numbers and I can give you a better answer.
Pitavastatin is 100% available in the US and insurers no longer require preauthorization. If you're over 40 it's free (no copay, by law) otherwise you just pay the usual deductible. If you have to pay cash for whatever reason, it $30/mo.
Now whether your primary care provider knows about it is another matter, lol. Buddy of mine got a prescription via telehealth. And while it only took five minutes (Sesame Health), the woman who wrote him the 90 day prescription said "I've been a cardiac nurse for 10 years and never heard of it, I looked it up and it sounds great, I can't believe this isn't prescribed more often".
Yes but rosuvastatin with bad kidney like mine can accumulate and then as a result rhabdo
yes in france pita doesn’t exist. I have pravastatin so its good.Yeah I see that's the "default" for severe chronic kidney disease, although Rosuvastatin is considered safe up to 10mg with CKD, even in dialysis patients,
FYI Pitavastatin has lower risk of muscle related sides in chronic kidney disease than Atorvastatin. Unlike Pitavastatin, Atorvastatin is metabolized by CYP3A4, and so are AAS, potentially causing a buildup of levels leading to muscle pain and rhabdo with simultaneous use of steroids.
Also Atorvastatin raises the risk of new onset diabetes higher than Rosu, and much higher than Pita, which actually improves rather than worsens insulin sensitivity.
Do you have a link to the FDA study looking at various ezetimibe dosages, I can't seem to find it?It's a reasonable option if ezetimibe is hard to get or costly, but that was a very small (240 patients) , short study done by the Veterans Administration looking to save money when it was expensive (90 tabs $1500 !!) and they didn't end up splitting.
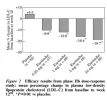
The FDA looked at much larger group, testing doses from .25mg to 40mg. They found that the benefit, in the vast majority, plateaued at 10mg.
Between 5 and 10mg LDL reduction on average was 16% and 19%, or 20% more reduction with 10mg. Bigger doses didn't lower LDL much more so they settled on 10mg as the standard.
Now as a generic it's only $14 for 90 x 10mg tablets in the US.
Do you have a link to the FDA study looking at various ezetimibe dosages, I can't seem to find it?
*Edit found it https://doi.org/10.1016/S1520-765X(01)90107-5
View attachment 346725
16% reduction at 5mg vs 19% reduction at 20mg. Hard to believe how effective even 0.25mg is. For example, with an LDL of 100, there is only a ~3 point reduction between 5 and 10mg of ezetimibe. I don't have a prescription and don't want any cholesterol drugs on my medical history right now, so I will stick with 5mg per day.
After a total of 5000 "LDL years" cumulative exposure, you'll have arteriosclerosis, So 50 years of average 100 LDL and you're at high risk of being on the operating table if you're lucky, or having a heart attack if you're not.

You give great information, and then just completely embellish this part. This is the reality:
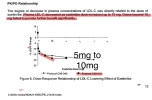
View attachment 346751
At 5000 at 50, you'd only have a 1% cumulative risk of a heart attack. If you extend the line out, mean age of heart attack would be around 75.
That's not to say you shouldn't get it under control now. The risk increases exponentially after 5000. But hitting 5000 is certainly not the death sentence it's being made out to be.
Yo Ghoul, what is a good maximum daily amount of saturated fat to reduce LDL. Is the AHA recommendation of less then 6% of total calories from saturated fat reasonable for AAS users, or should we strive for even less?Speaking of embellishment, I'm pretty sure I didn't say "death sentence" lol.
I'm curious where you found that chart.
The "5000mg" cumulative exposure is a great way to make it easy for people to grasp the concept of, as you pointed out, the way the threat is slow slow slow then starts to take off like a rocket,
A few updates regarding the cumulative risk numbers in the chart:
In the near decade since it was released, newer studies looking at larger pools of data along with the results of advanced imaging and autopsy results, reveal that the risk is substantially underestimated—2–3× higher for most adults, finding that nearly 60% of adults below the 5,000 mg·years threshold already have early atherosclerosis. As young as in their 20s.
Also, that chart uses an "average" level of risk factors. Anabolic steroid users have well above average risk factors, some obvious, ie, higher BP, others not completely understood, like the changes in heart tissue found in autopsies of young bodybuilders.
Anyway, it's great to see so many people interested in getting started earlier than the current reactive standard of dealing with lipids only once they've laid down a base of plaque for 40 years, and who see the obvious benefit of being proactive and stopping accumulation before it becomes an imminent threat. Those of us who started this later in life can only do a limited amount to reduce risk because of the accumulated damage.
Yo Ghoul, what is a good maximum daily amount of saturated fat to reduce LDL. Is the AHA recommendation of less then 6% of total calories from saturated fat reasonable for AAS users, or should we strive for even less?
Speaking of embellishment, I'm pretty sure I didn't say "death sentence" lol.
I'm curious where you found that chart.
I guess people don't die of heart attacks.
On this internets thing I have on my computer.
I've been on Lipitor for two decades. I'm currently off of Lipitor because it appears that Lipitor, after all these years, has started to injure my liver. That is a possible side effect. I'm actually generally for statins. (I'm not expert.) You shouldn't rely on my anecdotal experience as a reason for not taking a statin. Also, although the liver doctor thinks the statin is the most likely cause of my high liver enzymes (my ALT is 10 times the upper limit of normal), the cause still has not been determined. It's extremely rare for a person to have liver problems develop after many years on a statin not preceded by a dose increase. I want the cause to be the statin because then my liver would likely be fine so long as I don't take Lipitor. Whether I'd take another statin is another matter; my risk profile may have changed due to my weight loss and and the possibly greater risk of liver problems if I take another statin. My liver doctor said to stop taking reta (although he said it's probably not the cause) but to continue taking tirz. From what I've read, of the medicines I take, the second most likely to cause injury is the tirzepatide. (I should say third because reta hasn't been tried enough to obtain good data on the rate of liver injuries. Liver injury data tends to come after approval of drugs.)Doc wants to put me on a statin for my colesteral. Any of you guys on one and would you recommend it?
I've been on Lipitor for two decades. I'm currently off of Lipitor because it appears that Lipitor, after all these years, has started to injure my liver. That is a possible side effect. I'm actually generally for statins. (I'm not expert.) You shouldn't rely on my anecdotal experience as a reason for not taking a statin. Also, although the liver doctor thinks the statin is the most likely cause of my high liver enzymes (my ALT is 10 times the upper limit of normal), the cause still has not been determined. It's extremely rare for a person to have liver problems develop after many years on a statin not preceded by a dose increase. I want the cause to be the statin because then my liver would likely be fine so long as I don't take Lipitor. Whether I'd take another statin is another matter; my risk profile may have changed due to my weight loss and and the possibly greater risk of liver problems if I take another statin. My liver doctor said to stop taking reta (although he said it's probably not the cause) but to continue taking tirz. From what I've read, of the medicines I take, the second most likely to cause injury is the tirzepatide. (I should say third because reta hasn't been tried enough to obtain good data on the rate of liver injuries. Liver injury data tends to come after approval of drugs.)
Lower is better, true! In my country we have guidelines. But every cardiologist I know personally, even young ones with “normal” LDL, are self prescribing statins, to get low low, real low. Just saying.There's no rebound. You'll just return to where you were.
If Pita brings you below 55 you could skip the eze, And one less pill is always a noble goal.
However, there is no lower limit of LDL below which risk doesn't continue to decline. "Lower is better" is the unofficial motto of preventative cardiology.
And one other benefit to eze. Ezetimibe blocks cholesterol absorption in the intestines. Now most of what's being blocked, 80%+ is cholesterol produced in the liver, which dumps it into the intestines, then it's absorbed in the bloodstream (sounds weird I know, but that's how it works).
But the other 20% being blocked is dietary cholesterol. This gives you a little more "dietary flexibility", and the ability to eat saturated fats without them raising cholesterol as much as they otherwise would. So you could eat more red meat for instance without affecting your lipids as much.
Thanks for the reply, that is the same paper I was able to find and they had it on Sci-hub. The FDA approval page you linked was exactly what I was searching for, I hate how bad the search is on the FDA site.I've highlighted the LDL drop in 5 to 10mg doses found in the confirmatory protocol trial. Each square represents the doses used .25mg, 1mg, 2.5mg, 5mg, 10mg, 20mg (max). After 10mg you see it flattens out as it goes to 20mg with no further significant LDL reduction, but 5 to 10 shows a meaningful drop.
View attachment 346729
From this, the confidential drug approval response from the FDA. Some data is considered proprietary and redacted, but it's easy to extrapolate from the trial linked below.
(from clinical pharmacology review Part 1)
FDA Zetia Approval Docs
Here's the underlying trial used for the FDA application. I have a subscription that gives me access to (and can't see of its blocked to public view). If you can't read it lmk and I'll upload a copy here for you.
*It's worth noting a lot of "underpowered" papers came out chopping ezetimibe into smaller doses, as low as 2.5mg and concluding it was as effective as a full 10mg dose. Keep in mind this is when each tablet cost $50(!!!) so trying to get 4 for 1 made sense. Now that the price is 15¢, there's far less incentive to stray from the dose that's clinically proven to provide max benefit for the largest group of people.
Thanks for the reply, that is the same paper I was able to find and they had it on Sci-hub. The FDA approval page you linked was exactly what I was searching for, I hate how bad the search is on the FDA site.
I guess it was absurd
Got it, Reddit.
That chart comes from this paperSpeaking of embellishment, I'm pretty sure I didn't say "death sentence" lol.
I'm curious where you found that chart.
The "5000mg" cumulative exposure is a great way to make it easy for people to grasp the concept of, as you pointed out, the way the threat is slow slow slow then starts to take off like a rocket,
A few updates regarding the cumulative risk numbers in the chart:
In the near decade since it was released, newer studies looking at larger pools of data along with the results of advanced imaging and autopsy results, reveal that the risk is substantially underestimated—2–3× higher for most adults, finding that nearly 60% of adults below the 5,000 mg·years threshold already have early atherosclerosis. As young as in their 20s.
Also, that chart uses an "average" level of risk factors. Anabolic steroid users have well above average risk factors, some obvious, ie, higher BP, others not completely understood, like the changes in heart tissue found in autopsies of young bodybuilders.
Anyway, it's great to see so many people interested in getting started earlier than the current reactive standard of dealing with lipids only once they've laid down a base of plaque for 40 years, and who see the obvious benefit of being proactive and stopping accumulation before it becomes an imminent threat. Those of us who started this later in life can only do a limited amount to reduce risk because of the accumulated damage.

