Is there a difference between the Aromatase of T into E2(estradiol) between T
shots and T gels/cremes?
For instance some members, who are on T shots, recommend taking 0.25mg arimidex EOD or
every 3 days to keep E2 in the 20-30 range.
I'm on prescription T creme from LEF Rx Pharmacy 100mg T/day and I find that taking 0.25mg
Arimidex EOD or every three days stops my night/morn wood within 2 weeks. I am
now taking 0.25mg every week. I also take 50mg Zinc 2mg Copper every day and
400mg resveratrol every day so I don't know how much of an effect these vits
have in reducing aromatase of T into E2.
Anyone comments
There can be some marked differences in E2 production between topical and injectable. Reinforcing HeadDocs post, the treatment should be based on labs and not the rote administration of an aromatase inhibitor. My recommendation is to discontinue the AI unless the E2 levels are above 50. If they are, arimidex dose should be starting at 0.25 mg QOD.
One might think that there is an increase of E2 with topical administration since aromatase is found in the skin an adipose tissue. I do not find this to be the case. I can hardly recall a single person with E2 concern using transdermal testosterone.
From your post, it appears you are using a compounded treatment. Following are the abstracts and links to the full-text articles dealing with both forms of administration (compounded and brand name).
I should note that the finding of increased E2 levels with injectable T esters is a relatively common occurrence, particularly when the dose is 200 mg/week or more. Of course, the time between injection ad testing is a consideration.
Swerdloff RS, Wang C, Cunningham G, et al.
Long-Term Pharmacokinetics of Transdermal Testosterone Gel in Hypogonadal Men. J Clin Endocrinol Metab 2000;85(12):4500-10.
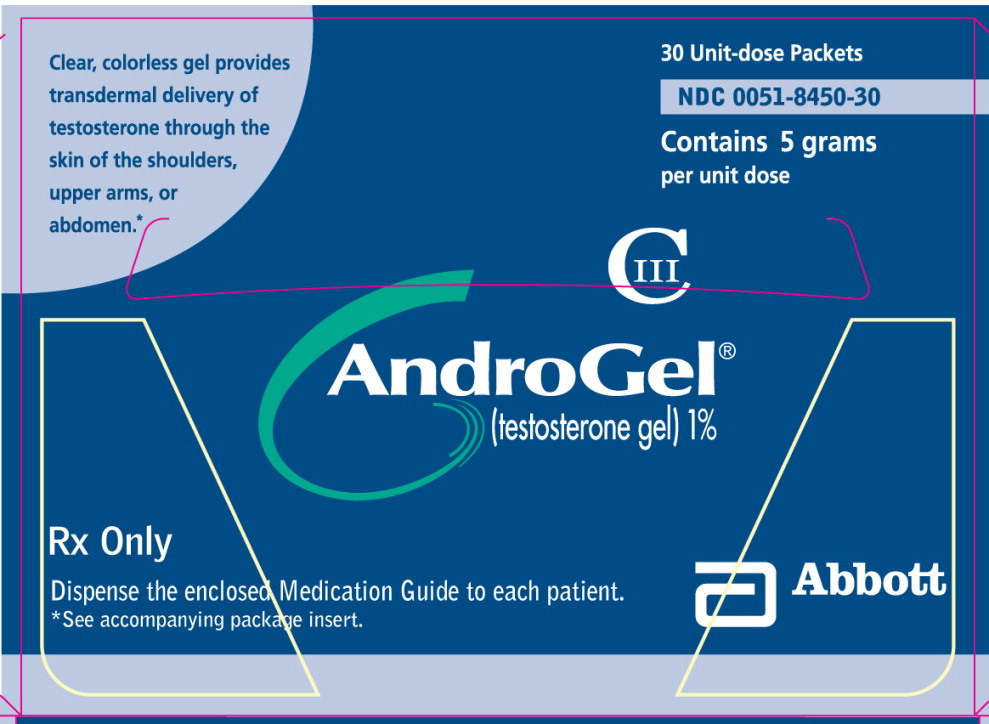
Transdermal delivery of testosterone (T) represents an effective alternative to injectable androgens. Transdermal T patches normalize serum T levels and reverse the symptoms of androgen deficiency in hypogonadal men. However, the acceptance of the closed system T patches has been limited by skin irritation and/or lack of adherence. T gels have been proposed as delivery modes that minimize these problems.
In this study we examined the pharmacokinetic profiles after 1, 30, 90, and 180 days of daily application of 2 doses of T gel (50 and 100 mg T in 5 and 10 g gel, delivering 5 and 10 mg T/day, respectively) and a permeation-enhanced T patch (2 patches delivering 5 mg T/day) in 227 hypogonadal men. This new 1% hydroalcoholic T gel formulation when applied to the upper arms, shoulders, and abdomen dried within a few minutes, and about 9-14% of the T applied was bioavailable. After 90 days of T gel treatment, the dose was titrated up (50 mg to 75 mg) or down (100 mg to 75 mg) if the preapplication serum T levels were outside the normal adult male range. Serum T rose rapidly into the normal adult male range on day 1 with the first T gel or patch application. Our previous study showed that steady state T levels were achieved 48-72 h after first application of the gel. The pharmacokinetic parameters for serum total and free T were very similar on days 30, 90, and 180 in all treatment groups. After repeated daily application of the T formulations for 180 days, the average serum T level over the 24-h sampling period (Cavg) was highest in the 100 mg T gel group (1.4- and 1.9-fold higher than the Cavg in the 50 mg T gel and T patch groups, respectively). Mean serum steady state T levels remained stable over the 180 days of T gel application. Upward dose adjustment from T gel 50 to 75 mg/day did not significantly increase the Cavg, whereas downward dose adjustment from 100 to 75 mg/day reduced serum T levels to the normal range for most patients. Serum free T levels paralleled those of serum total T, and the percent free T was not changed with transdermal T preparations. The serum dihydrotestosterone Cavg rose 1.3-fold above baseline after T patch application, but was more significantly increased by 3.6- and 4.6-fold with T gel 50 and 100 mg/day, respectively, resulting in a small, but significant, increase in the serum dihydrotestosterone/T ratios in the two T gel groups.
Serum estradiol rose, and serum LH and FSH levels were suppressed proportionately with serum T in all study groups; serum sex hormone-binding globulin showed small decreases that were significant only in the 100 mg T gel group. We conclude that transdermal T gel application can efficiently and rapidly increase serum T and free T levels in hypogonadal men to within the normal range. Transdermal T gel provided flexibility in dosing with little skin irritation and a low discontinuation rate.
Cutter CB.
Compounded percutaneous testosterone gel: use and effects in hypogonadal men. J Am Board Fam Pract 2001;14(1):22-32.
BACKGROUND: Current methods of testosterone replacement therapy are limited to fixed-dosage patches and depot injections. Neither of these methods provides ideal therapy because of the inflexibility of dosing and other nuisance problems associated with the patches and nonphysiologic hormone levels when depot injections are used. Testosterone gels offer the potential for convenience and ease of administration, as well as flexible dosing regimens, by means of a simple topical application. METHODS: Ten hypogonadal men were selected from the author's general practice, ranging in age from 44 to 77 years. Four of these men had newly diagnosed and 6 had preexisting hypogonadism. Patients were withdrawn from their previous hormone therapy (where applicable), and baseline laboratory studies were obtained for total testosterone, free testosterone, dihydrotestosterone, estradiol, luteinizing hormone, follicle-stimulating hormone, complete blood counts, lipid panels, and chemistry panels. The patients then started taking increasing dosages of the testosterone gel until physiologic levels of testosterone were realized or until the study period (6 weeks) was concluded. There was no blinding, and each patient served as his own control.
Testosterone and free testosterone levels were monitored weekly, and estradiol and dihydrotestosterone less frequently. At the conclusion of the study, all the baseline laboratory tests were repeated. A questionnaire evaluating the psychosexual well-being of the patients was administered before and after the treatment period. RESULTS: The average total testosterone level rose from 136 ng/dL to 442.9 ng/dL (P < .001). Average free testosterone levels rose from 34.2 pg/mL to 120.3 pg/mL (P < .001). Average dihydrotestosterone levels rose from 20.5 to 199.2 ng/dL (P = .006).
Average estradiol levels rose only slightly from 34.1 pg/mL to 40.0 pg/mL P = .191). Average total androgens (testosterone plus dihydrotestosterone) rose in all patients to therapeutic levels, from 149.3 ng/dL to 642.1 ng/dL (P = .001). The ratio of total androgen to estradiol rose from 5.1 to 17.1 (P < .002). Luteinizing hormone was suppressed in the 6 patients for whom meaningful data were available, and decreased on average from 5.66 to 1.10 mIU/mL (P = .005) Lipid effects were measured, and a 15% drop in all cholesterol fractions was noted (P < .005). Evaluation of the questionnaire showed considerable improvements in sexual function and overall well-being in all but 1 patient. No adverse effects or nuisance-problems were detected during the duration of the study. CONCLUSION: Topically applied testosterone gels are an effective and convenient means of hormone replacement in hypogonadal men.