@Type-IIx explains the benefits of GLP-1 and GIP agonists like Semaglutide and Tirzepatide, as true insulin sensitizing agents. how they are different from other weight loss drugs, and the benefits as partitioning agents for bodybuilders.
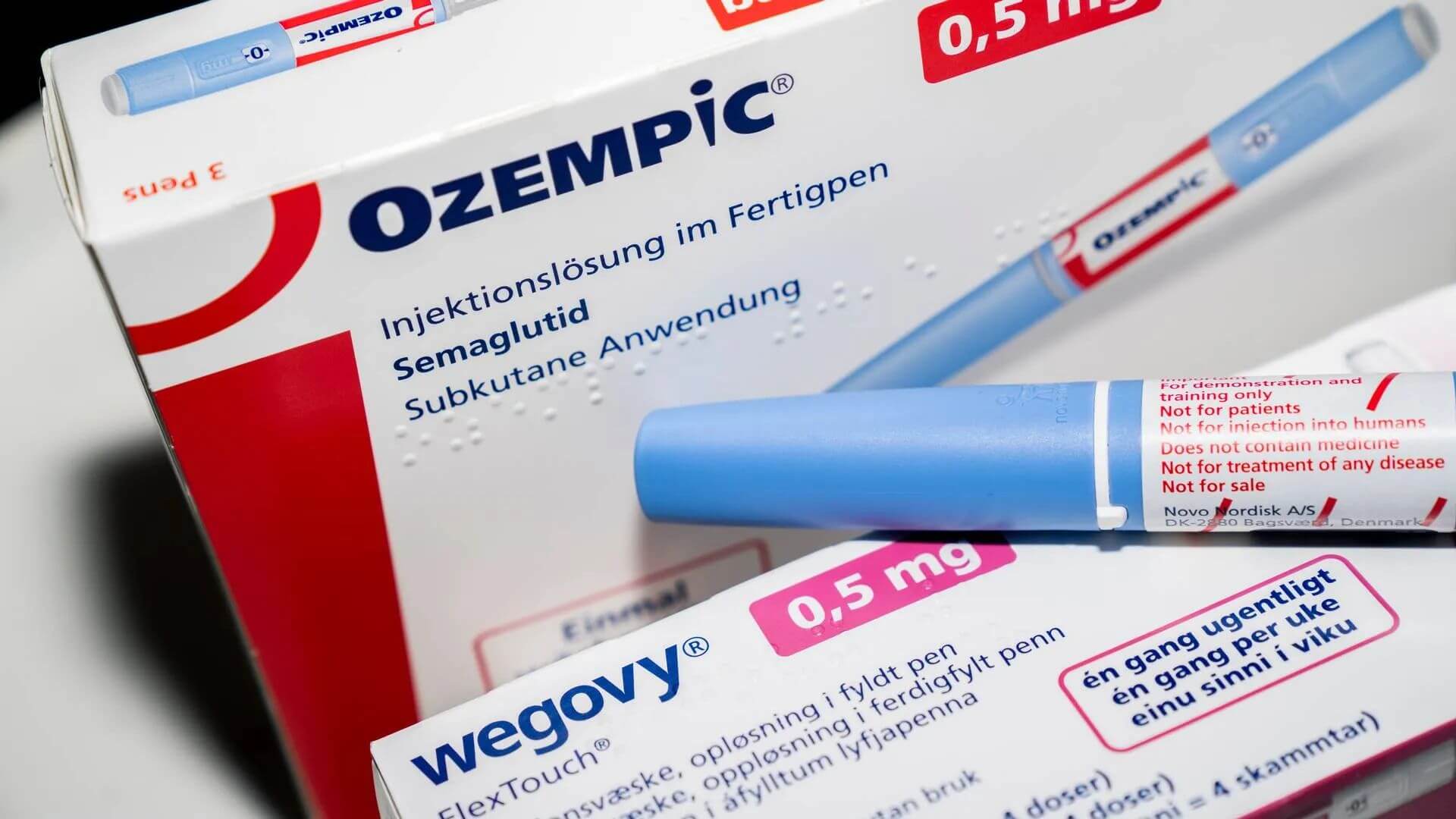
I'm sure you've read a lot about Ozempic, Wegovy, and Mounjaro for overweight sedentary people in the mainstream media but if you want to read about the use of these drug from a bodybuilding perspective, read on:
 thinksteroids.com
thinksteroids.com
I'm sure you've read a lot about Ozempic, Wegovy, and Mounjaro for overweight sedentary people in the mainstream media but if you want to read about the use of these drug from a bodybuilding perspective, read on:
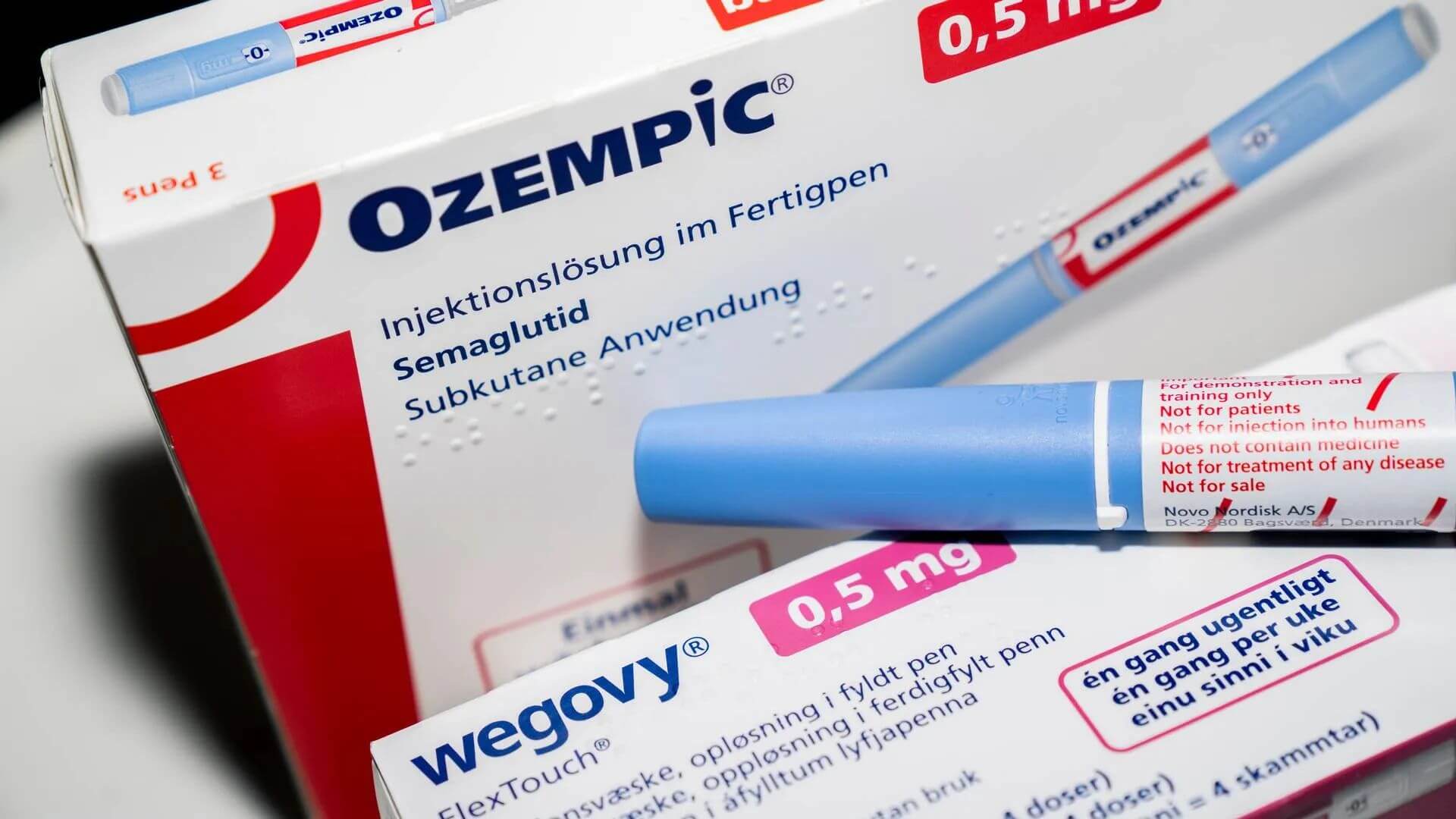
Semaglutide and Tirzepatide are More Than Just Weight Loss Drugs
Learn how GLP-1 and GIP agonists like Semaglutide and Tirzepatide enhance insulin sensitivity, preserve muscle mass and reduce fat stores.
 thinksteroids.com
thinksteroids.com

