As far as the former, I am guessing it was likely due to the number of forum members who stalked and harassed him from thread to thread, publicly and privately, over political issues. Dr. Scally never engaged or responded to them, yet they persisted. I miss him, and plan on inviting him back, hoping to see him return. Obviously, I will be disappointed if he doesn't but I would completely understand and honestly would not blame him. In hindsight, I should have done more to stop the harassment and feel a great deal of responsibility for not doing so.Why did Michael Scally MD and Dr JIM stop participating here?
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
Style variation
Guest viewing limit reached
- You have reached the maximum number of guest views allowed
- Please register below to remove this limitation
- Already a member? Click here to login
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
AAS and Cardiovascular/Pulmonary Function
- Thread starter Michael Scally MD
- Start date
KernelPanicFrenzy
New Member
If he writes the study without asking me more info, thats on him. I need them to get health care. If I get myself removed as a patient for using unregulated chinese peptides, I will be doing myself a disservice. So, Ill tread carefully.You are interfering with his personal ambitions.
If you introduce AAS, peptides, etc. it will likely compromise the prospects of a published case study.
Don't let that deter you from being honest with him - for the sake of scientific accuracy and disclosure. You are doing a disservice to the scientific community if you fail to disclose knowing that he will publish false information.
Any ideas why?Not because its actually bad for my condition, but because he has a dislike for TRT and GH in general.
I feel like 20 years ago, before the obesity crisis became such an epidemic, this was an easier view to hold. Then there's the whole wide world of transgender people. We should be entering a new world of hormones. Ah well, I'm pontificating.
KernelPanicFrenzy
New Member
His wife is an Endo, so she probably tells him about guys coming in with 500 testosterone wanting to be put on TRT? IDKAny ideas why?
I feel like 20 years ago, before the obesity crisis became such an epidemic, this was an easier view to hold. Then there's the whole wide world of transgender people. We should be entering a new world of hormones. Ah well, I'm pontificating.
I think using testosterone to maximize performance has been demonized, and it still is, but I think it shouldn't be.
Has nothing to do with transgenders. That is not TRT.
Eddie.
Member
I’ve been involved in this game and using PED’s for the better part of 25 years. I get regular blood work and have been open with my use to my doctors. Here’s been my experience.
I have a bad history of heart disease and issues on my father’s side. My father was a competitive bodybuilder and used AAS back in the 80’s. He died at age 37 due to cardiomyopathy. Now his father, who never touched a steroid, or worked out for that matter, died of a heart attack at 42.
My first heart issue came in the form of pericarditis, an inflammation of the outer protective sheath of the heart. Felt like I was having a heart attack. I do believe this was steroid induced. This resulted in regular blood work and heart exams due to my family history.
Over the years I’ve had progressing left ventricle hyperteophy. It started as mild and progressed to moderate borderline severe. This has been measured by multiple echocardiograms over the years. It has taken 20 years to progress from mild to high moderate. However, my heart function is not affected.
I also have a faulty aeortic valve, but this is hereditary per my cardiologist. So, I have a combination of “heart issues” some possibly attributed to AAS use over the years and some genetic.
Based on my family history I had no expectation of living past 40 but despite these issues, I’m 53 and going strong and have been running gear for 25 years. However, my doses and the compounds I can tolerate have decreased year over year for the past 10 years or so.
I have a bad history of heart disease and issues on my father’s side. My father was a competitive bodybuilder and used AAS back in the 80’s. He died at age 37 due to cardiomyopathy. Now his father, who never touched a steroid, or worked out for that matter, died of a heart attack at 42.
My first heart issue came in the form of pericarditis, an inflammation of the outer protective sheath of the heart. Felt like I was having a heart attack. I do believe this was steroid induced. This resulted in regular blood work and heart exams due to my family history.
Over the years I’ve had progressing left ventricle hyperteophy. It started as mild and progressed to moderate borderline severe. This has been measured by multiple echocardiograms over the years. It has taken 20 years to progress from mild to high moderate. However, my heart function is not affected.
I also have a faulty aeortic valve, but this is hereditary per my cardiologist. So, I have a combination of “heart issues” some possibly attributed to AAS use over the years and some genetic.
Based on my family history I had no expectation of living past 40 but despite these issues, I’m 53 and going strong and have been running gear for 25 years. However, my doses and the compounds I can tolerate have decreased year over year for the past 10 years or so.
KernelPanicFrenzy
New Member
Take a look at tirzepatide. It's been shown now to shrink heart cells. It reversed my aortic stenosis.I’ve been involved in this game and using PED’s for the better part of 25 years. I get regular blood work and have been open with my use to my doctors. Here’s been my experience.
I have a bad history of heart disease and issues on my father’s side. My father was a competitive bodybuilder and used AAS back in the 80’s. He died at age 37 due to cardiomyopathy. Now his father, who never touched a steroid, or worked out for that matter, died of a heart attack at 42.
My first heart issue came in the form of pericarditis, an inflammation of the outer protective sheath of the heart. Felt like I was having a heart attack. I do believe this was steroid induced. This resulted in regular blood work and heart exams due to my family history.
Over the years I’ve had progressing left ventricle hyperteophy. It started as mild and progressed to moderate borderline severe. This has been measured by multiple echocardiograms over the years. It has taken 20 years to progress from mild to high moderate. However, my heart function is not affected.
I also have a faulty aeortic valve, but this is hereditary per my cardiologist. So, I have a combination of “heart issues” some possibly attributed to AAS use over the years and some genetic.
Based on my family history I had no expectation of living past 40 but despite these issues, I’m 53 and going strong and have been running gear for 25 years. However, my doses and the compounds I can tolerate have decreased year over year for the past 10 years or so.
I'd also look into Ss-31 "Elamipretide"
Last edited:
Ghoul
Member
Take a look at tirzepatide. It's been shown now to shrink heart cells. It reversed my aortic stenosis.
I'd also look into Ss-31 "Elamipretide"
I was just about to mention this.
Tirz has been shown to reverse left ventricular hypertrophy via mechanisms apart from weight loss alone.
"Kramer, a cardiovascular imager, also led a magnetic resonance imaging substudy looking at how tirzepatide, sold under the brand name Zepbound, affected recipients’ heart structure and function. The researchers found beneficial reductions in both left ventricular mass (weight of the heart) and in the amount of surrounding fat tissue. The reduction in LV mass correlated with the reduction in body weight, as well as with decreases in left ventricular volumes.
“This drug is reversing the abnormal properties of the heart brought on by obesity,” Kramer said. “There is much more to these drugs than weight loss alone.”
In other words, LV Hypertrophy brought on by stress, in this case obesity, is being reversed. I'm sure I've seen another study that showed the improvement was even greater in normal weight subjects, a rarity, as so little of the massive amount of research going on into GLPs involves normal weight or non-diabetic subjects.
Weight-Loss Drug Tirzepatide Reduces Heart Failure Deaths
Tirzepatide, from pharmaceutical company Eli Lilly and Co., was tested in the SUMMIT clinical trial at 146 sites in the United States and abroad.
There's a link between endotoxin exposure and heart remodeling, and Tirz appears to affect that pathway to stop progressive worsening of the condition, and even reverses it.
MyNameIsJeff
Member
Sounds more like the LV mass reduction was a function of reduced body mass and improvements to concomitant metabolic syndrome.Tirz has been shown to reverse left ventricular hypertrophy via mechanisms apart from weight loss alone.
"Kramer, a cardiovascular imager, also led a magnetic resonance imaging substudy looking at how tirzepatide, sold under the brand name Zepbound, affected recipients’ heart structure and function. The researchers found beneficial reductions in both left ventricular mass (weight of the heart) and in the amount of surrounding fat tissue. The reduction in LV mass correlated with the reduction in body weight, as well as with decreases in left ventricular volumes.
I would have to see such a study before I buy in the hype of GLP-1 agonists for use in the non-obese.I'm sure I've seen another study that showed the improvement was even greater in normal weight subjects, a rarity, as so little of the massive amount of research going on into GLPs involves normal weight or non-diabetic subjects.
I’m with you, however I couldn’t resist and began using Retatrutide almost two weeks ago. I can see why this stuff works because I definitely notice a moderate reduction in my appetite. The only downside is higher resting heart rate.Sounds more like the LV mass reduction was a function of reduced body mass and improvements to concomitant metabolic syndrome.
I would have to see such a study before I buy in the hype of GLP-1 agonists for use in the non-obese.
Please tell me more about the aortic stenosis reversal. Any other changes in your echocardiogram? How bad was it before compared to now? Mild, moderate, severe? I have aortic regurgitation so I am very interested in this.Take a look at tirzepatide. It's been shown now to shrink heart cells. It reversed my aortic stenosis.
I'd also look into Ss-31 "Elamipretide"
KernelPanicFrenzy
New Member
They haven't done a follow up echo. I was meeting with the surgeon on 9/4 to schedule my surgery. It was bad enough they did not want to wait. I had a 10-20% chance of dying on the table and a very hard recoveryPlease tell me more about the aortic stenosis reversal. Any other changes in your echocardiogram? How bad was it before compared to now? Mild, moderate, severe? I have aortic regurgitation so I am very interested in this.
Symptoms were bad, I couldn't walk into Safeway without needing a rest. Didn't have the breath to put the cart in the cart return. This was in june when it started
By the time I met the surgeon I was able to cut up multiple logs with a chainsaw, throw the rounds and split with a splitter. Walk around Costco for an hour without issue.
They told me surgery was the only option.
Unless symptoms return, I go back for an echo late February I'll post both before and after echos
Same here. I have some stenosis and regurgitation due to a bicuspid vs. tricuspid valve flap (for lack of a more proper term), thus the genetic component, that causes some mild regurgitation. My doc has advised I will likely need to get it replaced at some point over the next 5-10 years, this the annual echo.Please tell me more about the aortic stenosis reversal. Any other changes in your echocardiogram? How bad was it before compared to now? Mild, moderate, severe? I have aortic regurgitation so I am very interested in this.
Wow, that’s really impressive. I am very curious to see how the stenosis is doing since it’s not really supposed to be reversible. You’ll probably still need the valve replaced eventually but it sounds like you’ve delayed it. Honestly, getting the valve replaced isn’t really a big deal these days. You can get a minimally invasive procedure and be out of the hospital the next day. The valves last 10-15 years now if you don’t get a mechanical valve (which lasts a lifetime but then you have to be on Warfarin for life).They haven't done a follow up echo. I was meeting with the surgeon on 9/4 to schedule my surgery. It was bad enough they did not want to wait. I had a 10-20% chance of dying on the table and a very hard recovery
Symptoms were bad, I couldn't walk into Safeway without needing a rest. Didn't have the breath to put the cart in the cart return. This was in june when it started
By the time I met the surgeon I was able to cut up multiple logs with a chainsaw, throw the rounds and split with a splitter. Walk around Costco for an hour without issue.
They told me surgery was the only option.
Unless symptoms return, I go back for an echo late February I'll post both before and after echos
KernelPanicFrenzy
New Member
If its an option. I had a TAVR attempted before my last surgery and it failed. The Dr who did my first couple surgerys is the one who developed the techniqueWow, that’s really impressive. I am very curious to see how the stenosis is doing since it’s not really supposed to be reversible. You’ll probably still need the valve replaced eventually but it sounds like you’ve delayed it. Honestly, getting the valve replaced isn’t really a big deal these days. You can get a minimally invasive procedure and be out of the hospital the next day. The valves last 10-15 years now if you don’t get a mechanical valve (which lasts a lifetime but then you have to be on Warfarin for life).
Yes they told me it was irreversible without surgery, but believe I reversed it, if I get to my goal weight, he thinks I might be able to avoid the surgery table altogether, maybe.
KernelPanicFrenzy
New Member
I was going to have these done in one surgery
Subaortic Stenosis (SubAS): This involved a resection to alleviate the obstruction caused by the subaortic membrane.
Left Ventricular Outflow Tract (LVOT) Enlargement.
Aortic Valve Replacement.
Aortic Root Replacement.
Right Ventricle to Pulmonary Artery (RV-PA) Conduit Replacement.
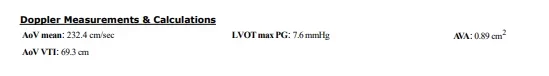
Below is more info on it if you are curious. Ill post the followup echo when I have it.
CARDIAC STUDIES
Traneseophageal echocardiogram (7/29/2024, UWMC)
History of coarctation of aorta and subaortic/aortic stenosis s/p Ross and
PVR. TEE for evaluation of subaortic/aortic stenosis. Underlying rhythm
sinus.
Flow acceleration in left ventricular outflow tract with cross-sectional LVOT
area of 1.9 cm2 by planimetry due to presence of subaortic membrane. Note
that this may be an overestimate of the area due to difficult of obtaining a
true cross-section. Anterograde flows with max velocity 3.5 m/s, mean
gradient 26mmHg with focal step-up in LVOT suggestive of significant
moderate-severe subaortic stenosis.
S/p Ross procedure with trileaflet neoaortic valve. Anterograde hemodynamics
difficult to assess in setting of subvalvular stenosis.
Mitral valve structurally normal with trace eccentric regurgitation.
Tricuspid valve structurally normal with trace regurgitation.
Bioprosthetic pulmonic valve not well-seen.
Left ventricle grossly normal in size with moderate concentric hypertrophy.
Normal systolic function without regional wall motion abnormalities.
Right ventricle normal in size and systolic function.
Dilated ascending aortat (4.5 cm).
No pericardial effusion.
Compared to TTE 6/12/2024, LVOT/aortic velocities measure lower on today's
study. Clear subvalvular aortic stenosis now identified. Pulmonic valve not
assessed on today's study.
Patch monitor (6/17/2024, UWMC)
- Predominant rhythm: NSR
- Atrial Tachycardia (AT) 192 episodes, Longest 11.5 m @ Avg 153 bpm up to 197 bpm, Fastest 2.4 m @ Avg 166 bpm up to 201 bpm
- PAC 2.3 %
- PVC <0.1 %
CATH 10/27/2023
The right heart catheter was advanced across the RV to PA conduit and bioprosthesis and into the left pulmonary capillary wedge position. The left heart catheter was advanced across the left aortic arch, prolapsed across the neoaortic valve, and advanced into the left ventricle.
- Catheter course:
PA 68%, RFA 93%. Qp/Qs assumed to be 1.0. Systemic Fick cardiac output/index 5.68/2.39. PVR 1.94 Wood units. SVR 12.5 Wood units.
- Oximetry:
RA 10, RV 66/11, distal MPA 39/17/27, LPA 39/16/25, L PCW, LV 133/21, ascending aorta 106/60/80, descending aorta 109/60/81.
- Pressures:
A. Selective right coronary artery angiography reveals a nondominant right coronary artery arising from the right coronary cusp. The surgically reimplanted ostium is widely patent. The right coronary artery gives rise to 1 very high acute marginal artery. The right coronary artery continues within the atrioventricular groove as an atretic vessel providing no substantial additional branches.
- Angiography:
B. Selective left circumflex coronary angiography reveals a large dominant vessel arising off the left coronary cusp from its own ostium. The left circumflex gives rise to multiple posterolateral branches and a posterior descending artery. Angiographically normal.
C. Selective left anterior descending artery angiography reveals a large vessel arising off its own ostium adjacent to the left circumflex coronary artery. There is an 80% relative narrowing of the ostial left anterior descending artery. The remainder of the vessel is free from obstruction and is otherwise angiographically normal.
Assessment and Plan:
Patient has now undergone invasive hemodynamics revealing mildly elevated right and left-sided filling pressures, a modest 27 mmHg gradient across the RV to PA conduit and bioprosthesis, a mild to moderate 27 mmHg gradient across the left ventricular outflow tract, and no gradient between the a sending and descending aorta. Overall these findings are consistent with the patient's recent imaging showing no evidence of severe left or right outflow tract obstruction. Additional findings include a cardiac index that is mildly depressed at 2.4 L/min/m², high normal pulmonary vascular resistance, and normal systemic vascular resistance. Selective coronary angiography revealed a left anterior descending arising off its own ostium with a relative 70 to 80% stenosis. This was further investigated with a pressure wire revealing an IFR nadir of 0.99 consistent with a hemodynamically insignificant lesion. There is no overt evidence of a cardiac cause for the patient's more recent dyspneic symptoms based on this study.
ASSESSMENT
Patient is an 38 year old male with coarctation of the aorta s/p subclavian flap repair, multilevel LVOT obstruction s/p multiple subAS resections and Ross procedure with RV-PA conduit replacement in 2009 seen in Cardiology clinic for follow up.
With improvement in his symptoms following his significant weight loss on tirzepatide, we agree with continued deferment of cardiac surgery.
He is continuing to take testosterone at the current time. He had discussed this with DR at his last visit but elected to continue, particularly in light of the immense improvement in symptoms he is experiencing.
We discussed the need for ongoing surveillance of left ventricular outflow tract gradients. Will see him back in a couple of months with a transthoracic echo to look at left ventricular outflow tract gradients. We encouraged him to increase aerobic activity. He is going to stop creatine supplements.
- Encouraged ongoing weight loss with his appetite
- No changes to medical therapy today other than stopping creatine
- Follow-up next available slot with Dr. or myself with an echocardiogram to look at left ventricular outflow tract gradients
- CTA reviewed, no hemodynamically significant recoarctation
- Blood pressure and the right arm adequately controlled currently



I dont know. I liked Jim and he was a fun loving jackass in his own right. I never thought he was bullied into submission. Perhaps we were all unaware of any private matters spilling over. As far as Scally goes, he ripped ass PRN and always rightfully so. The real Scally that is... Only his screen name has remained for some time. I only chimed in on this one because I was disappointed to see you second guess yourself. Meso was founded on Freedom first, and demanding intelligence to wield it. Desire to learn was the minimum requirement. And those that abused the freedom were quickly humbled and could either profit by it or die off. I took my share of hits on the learning curve and appreciated every one of them.As far as the former, I am guessing it was likely due to the number of forum members who stalked and harassed him from thread to thread, publicly and privately, over political issues. Dr. Scally never engaged or responded to them, yet they persisted. I miss him, and plan on inviting him back, hoping to see him return. Obviously, I will be disappointed if he doesn't but I would completely understand and honestly would not blame him. In hindsight, I should have done more to stop the harassment and feel a great deal of responsibility for not doing so.
Just saying. We all make our share of mistakes, don't add another one to the fire by second guessing the things you did right too... I was a loose cannon and in my opinion you were well tempered and just what the board called for and you know this. I miss my Meso days but I can never engage again as in the past. The internet is just so full of ghosts and ghouls it becomes disheartening. Seeing you have to change your position to hall cop over this over the years is troubling. But Kudos regardless you do what you must we know.
dutchtowner
New Member
Hope you have a good update. I have my next echo in April. I got stenosis, and my younger brother just had TAVR with good results. Doc says I may need it but wait and see progession. I plan to research tirz a bit more and started taking a bit of K2 to send calcium where it needs to be.
I was going to have these done in one surgery
Subaortic Stenosis (SubAS): This involved a resection to alleviate the obstruction caused by the subaortic membrane.
Left Ventricular Outflow Tract (LVOT) Enlargement.
Aortic Valve Replacement.
Aortic Root Replacement.
Right Ventricle to Pulmonary Artery (RV-PA) Conduit Replacement.
Below is more info on it if you are curious. Ill post the followup echo when I have it.
View attachment 305780
View attachment 305781
View attachment 305782
View attachment 305783
KernelPanicFrenzy
New Member
Had my follow-up the other day. My heart has improved in every measure. May have slightly decreased narrowing, but wasn't definitive. Didn't progress tho, and no symptoms.
This was while also using test/primo/HGH/proviron also introduced super shred.
Started taking telmisartan on my own from India.
Best of luck
I was a test subject for the TAVR but wasn't a candidate
This was while also using test/primo/HGH/proviron also introduced super shred.
Started taking telmisartan on my own from India.
Best of luck
I was a test subject for the TAVR but wasn't a candidate
justtrtbro
Member
One of a few reasons I started 2.5mg once weekly a few weeks ago.Take a look at tirzepatide. It's been shown now to shrink heart cells. It reversed my aortic stenosis.
I'd also look into Ss-31 "Elamipretide"
I've been on 100mg/wk of TRT for exactly one year yesterday though, so hopefully any heart issues will develop slowly, or be balanced out with tirz use over the long run.
Similar threads
- Replies
- 19
- Views
- 861
- Replies
- 64
- Views
- 3K
- Replies
- 4
- Views
- 813
Sponsors
Latest posts
-
-
MESO-Rx Sponsor PCT 24X7 "1 stop shop for all day healthcare"
- Latest: twistedfire11
-
-

